(2/x) The first step is identifying pts. at highest risk of hemodynamic collapse.
Anyone who is critically ill is at risk, however, these are some particular cases that I think are the highest risk:
1. Pt. with shock (mottled, poor cap refill, hypotension)
2. LV/RV dysfunction (acute or chronic)
3. Pericardial Effusions (even without tamponade)
4. Pulmonary HTN (yikes)
5. Lobar Collapse (these pts. often tank pressure)
6. High catecholamine drive (respiratory distress etc.)
For these patients, take a few extra moments to prepare.
Anyone who is critically ill is at risk, however, these are some particular cases that I think are the highest risk:
1. Pt. with shock (mottled, poor cap refill, hypotension)
2. LV/RV dysfunction (acute or chronic)
3. Pericardial Effusions (even without tamponade)
4. Pulmonary HTN (yikes)
5. Lobar Collapse (these pts. often tank pressure)
6. High catecholamine drive (respiratory distress etc.)
For these patients, take a few extra moments to prepare.
(3/x) Next is deciding the urgency of intubation. Each patient has a competing risk of dying from lack of intubation (Airway and Breathing) vs. circulatory collapse (circulation).
Sometimes you are simply stuck, for example, a massive GI bleed with imminent airway loss and severe hypotension.
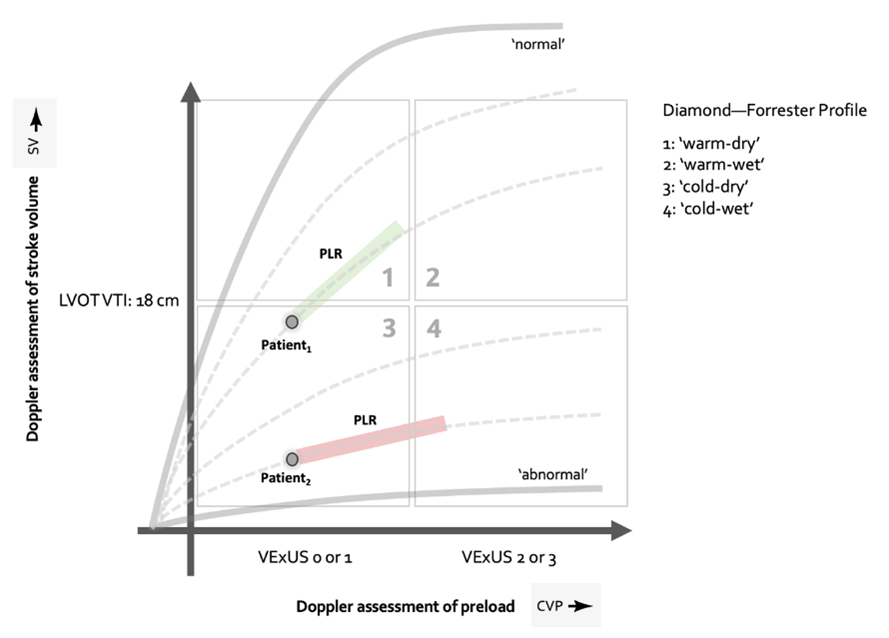
Other patients you have time to resuscitate, then intubate. As part of this resuscitation, phenotype the etiology of shock (if you haven't).
Then, optimize their shock management for a bit.
E.g. blood/volume resuscitation, pressors, inotropes, inhaled pulmonary vasodilators etc.
Sometimes you are simply stuck, for example, a massive GI bleed with imminent airway loss and severe hypotension.
Other patients you have time to resuscitate, then intubate. As part of this resuscitation, phenotype the etiology of shock (if you haven't).
Then, optimize their shock management for a bit.
E.g. blood/volume resuscitation, pressors, inotropes, inhaled pulmonary vasodilators etc.
(4/x) Next, prepare the right equipment.
1. Monitors - arterial lines super valuable for shock intubations.
2. Induction Drugs - appropriately dosed anesthetic (lower) + paralytics (higher)
3. Vasoactive medications - I like to have norepinephrine hooked up and running for all of these patients
4. Push dose vasopressors (phenyl, epi, vaso etc. as appropriate based on shock type). My general approach.
Cardiogenic - epi
Pulm HTN/RV - epi/vaso
Distributive - Phenyl/Vaso
5. The right team (RNs, RTs, MDs etc.)
6. The right setting. If time permits, intubating in a resuscitative setting (OR, ED, ICU vs. ward is best)
1. Monitors - arterial lines super valuable for shock intubations.
2. Induction Drugs - appropriately dosed anesthetic (lower) + paralytics (higher)
3. Vasoactive medications - I like to have norepinephrine hooked up and running for all of these patients
4. Push dose vasopressors (phenyl, epi, vaso etc. as appropriate based on shock type). My general approach.
Cardiogenic - epi
Pulm HTN/RV - epi/vaso
Distributive - Phenyl/Vaso
5. The right team (RNs, RTs, MDs etc.)
6. The right setting. If time permits, intubating in a resuscitative setting (OR, ED, ICU vs. ward is best)
(5/x) Be generous with with vasoactive medications peri-intubation, and remember, most arrests happen 5-10minutes after induction NOT immediately.
Don't celebrate too early. x.com
Don't celebrate too early. x.com
(6/x) Most importantly, recognize that intubation almost certainly did NOT fix their shock!
Now is the hard part. Phenotype the type of shock, diagnose the cause, and treat the underlying cause and complications.
What other PEARLS are there here? x.com
Now is the hard part. Phenotype the type of shock, diagnose the cause, and treat the underlying cause and complications.
What other PEARLS are there here? x.com
Loading suggestions...