(1/x) The term 'pre-renal' acute kidney injury is dated and should stop being taught in medical schools.
Why? The term pre-renal is inextricably linked to the idea that the treatment of pre-renal AKI is IV fluids.
Here's the paradigm of hemodynamic AKI and why it is helpful.
A 🧵
#foamed #medtwitter #meded #hemodynamics
Why? The term pre-renal is inextricably linked to the idea that the treatment of pre-renal AKI is IV fluids.
Here's the paradigm of hemodynamic AKI and why it is helpful.
A 🧵
#foamed #medtwitter #meded #hemodynamics
(2/x) Now most of us were taught this approach to AKI in medical school 🏫
Pre-renal AKI
Renal AKI
Post-renal AKI
Conceptually, it works really well for the renal and post renal, however, pre-renal is an imprecise term that misleads many people ❌
Now before people say 'well of course pre-renal AKI doesn't mean fluids as treatment, it can be cardiorenal etc. etc...' I ask junior residents every month in the ICU what the treatment of pre-renal AKI is an 80% of them respond back with IV fluids.
For experts, the terminology is less important. For trainees, it is crucial.
Here is why I think we should start teaching and using the following approach to AKI.
Hemodynamic AKI
Renal AKI
Post Renal AKI
Pre-renal AKI
Renal AKI
Post-renal AKI
Conceptually, it works really well for the renal and post renal, however, pre-renal is an imprecise term that misleads many people ❌
Now before people say 'well of course pre-renal AKI doesn't mean fluids as treatment, it can be cardiorenal etc. etc...' I ask junior residents every month in the ICU what the treatment of pre-renal AKI is an 80% of them respond back with IV fluids.
For experts, the terminology is less important. For trainees, it is crucial.
Here is why I think we should start teaching and using the following approach to AKI.
Hemodynamic AKI
Renal AKI
Post Renal AKI
(3/x) When we discuss pre-renal AKI, we are really discussing hemodynamic contributors to AKI (that can potentially be modified through hemodynamic intervention)
These include:
1) Hypovolemia (or more broadly, low mean systemic filling pressure)
2) Inadequate MAP (distributive) - e.g. some pts. autoregulate at higher MAPs
3) Venous Congestion (congestive injury is caused by reduction in renal perfusion pressure which approximates MAP - CVP with caveats below)
4) Low stroke volume from cardiac dysfunction (e.g. cardiogenic or obstructive shock)
Let's dive deep into each of these.
These include:
1) Hypovolemia (or more broadly, low mean systemic filling pressure)
2) Inadequate MAP (distributive) - e.g. some pts. autoregulate at higher MAPs
3) Venous Congestion (congestive injury is caused by reduction in renal perfusion pressure which approximates MAP - CVP with caveats below)
4) Low stroke volume from cardiac dysfunction (e.g. cardiogenic or obstructive shock)
Let's dive deep into each of these.
(4/x) Hypovolemic AKI (or even better, low mean systemic filling pressure [Pmsf]).
True hypovolemia from something like hemorrhage is an obvious cause of AKI. If someone is bleeding, give them blood. This will improve their hypovolemic AKI.
For patients in hospital, most pts. are not truly hypovolemic (some post surgical etc. are). Many, however, have low filling pressures (Pmsf) which make them behave hypovolemic.
Venous return is driven by the difference between mean systemic filling pressure and right atrial pressure. Giving IV fluids can increase Pmsf , but so can increasing venous tone through vasopressors.
This means, some 'hypovolemic' behaving patients can have their stroke volume restored with vasopressors instead of IV fluids. In some cases, there can be an advantage to this.
For example, every extra bolus of fluid given to a patient needs to be 'paid off' eventually. Kind of like a credit card where you can use it to purchase something, but the debt need to be paid off.
If you can achieve the same restoration of stroke volume using vasopressors to improve Pmsf, this might be beneficial as it can prevent overload.
Now obviously this is complex and I understand that vasopressors are not available in every hospital unit, but broadening our understanding of the interplay between Pmsf and venous return is helpful.
True hypovolemia from something like hemorrhage is an obvious cause of AKI. If someone is bleeding, give them blood. This will improve their hypovolemic AKI.
For patients in hospital, most pts. are not truly hypovolemic (some post surgical etc. are). Many, however, have low filling pressures (Pmsf) which make them behave hypovolemic.
Venous return is driven by the difference between mean systemic filling pressure and right atrial pressure. Giving IV fluids can increase Pmsf , but so can increasing venous tone through vasopressors.
This means, some 'hypovolemic' behaving patients can have their stroke volume restored with vasopressors instead of IV fluids. In some cases, there can be an advantage to this.
For example, every extra bolus of fluid given to a patient needs to be 'paid off' eventually. Kind of like a credit card where you can use it to purchase something, but the debt need to be paid off.
If you can achieve the same restoration of stroke volume using vasopressors to improve Pmsf, this might be beneficial as it can prevent overload.
Now obviously this is complex and I understand that vasopressors are not available in every hospital unit, but broadening our understanding of the interplay between Pmsf and venous return is helpful.
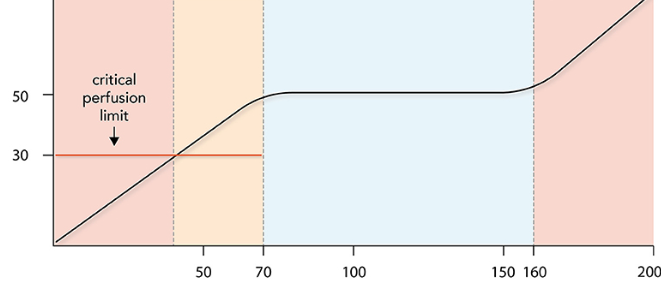
(5/x) Inadequate MAP (distributive)
I think of this cause of hemodynamic AKI in patients who tend to autregulate at higher blood pressures chronically, but have lower MAPs due to acute illness.
E.g. chronic hypertensive patient who lives with MAP of 110mmHg is in the ICU with MAP of 65mmHg and not peeing. In some of these patients, a MAP challenge (increase MAP to 80mmHg for 6 hours) can be useful.
If the patient increases their urine output significantly, this can be a sign that the MAP of 65mmHg was not adequate for them.
I don't find that this is a particularly common cause of AKI, but is worth considering in patients who other maneuvers fail.
I think of this cause of hemodynamic AKI in patients who tend to autregulate at higher blood pressures chronically, but have lower MAPs due to acute illness.
E.g. chronic hypertensive patient who lives with MAP of 110mmHg is in the ICU with MAP of 65mmHg and not peeing. In some of these patients, a MAP challenge (increase MAP to 80mmHg for 6 hours) can be useful.
If the patient increases their urine output significantly, this can be a sign that the MAP of 65mmHg was not adequate for them.
I don't find that this is a particularly common cause of AKI, but is worth considering in patients who other maneuvers fail.
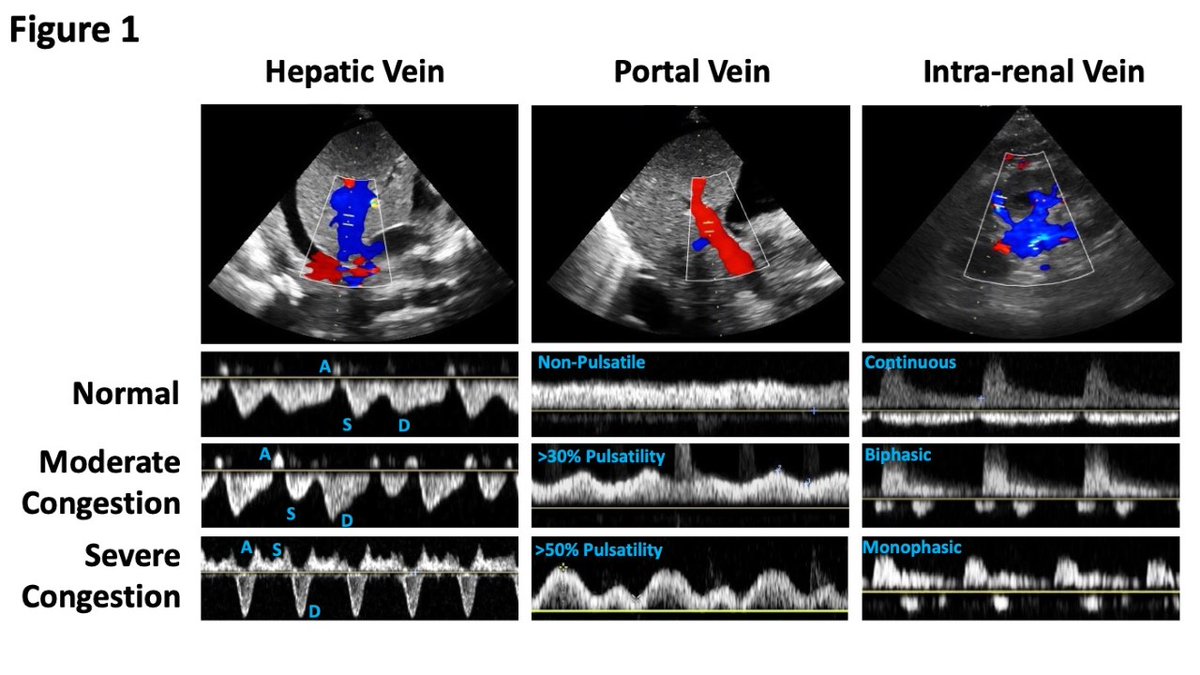
(6/x) Venous Congestion induced AKI 🫘💧
Everyone organ has a perfusion pressure.
For the kidney, this can be approximated by MAP - CVP. When the MAP drops in the ICU, we defend it aggressively with vasopressors / fluids. When the CVP rises we... well often ignore it despite the fact it can impact renal perfusion.
Unfortunately, CVP alone is not adequate to predict organ level congestion (I will discuss more in another thread), but assessing for venous congestion at the organ level using Doppler (e.g. renal Doppler, portal vein, hepatic vein, IJ, femoral vein) is valuable as patients with congestions may benefit from cardiac support with inotropes or diuresis (depending on the cause of congestion).
Everyone organ has a perfusion pressure.
For the kidney, this can be approximated by MAP - CVP. When the MAP drops in the ICU, we defend it aggressively with vasopressors / fluids. When the CVP rises we... well often ignore it despite the fact it can impact renal perfusion.
Unfortunately, CVP alone is not adequate to predict organ level congestion (I will discuss more in another thread), but assessing for venous congestion at the organ level using Doppler (e.g. renal Doppler, portal vein, hepatic vein, IJ, femoral vein) is valuable as patients with congestions may benefit from cardiac support with inotropes or diuresis (depending on the cause of congestion).
(7/x) Low stroke volume from cardiac dysfunction (cardiogenic or obstructive).
I used to think of this as cardiogenic shock, however, cardiogenic shock induces renal dysfunction from both low stroke volume and congestion. To be more precise, I try to think of this as poor forward flow from cardiac dysfunction.
These patients need to have the underlying cause treated, and then consider RV, LV, supportive therapy with inotropes, inodilators, vasodilators etc.
This is a rare phenotype for most ward patients, but is something we encounter regularly in the ICU.
I used to think of this as cardiogenic shock, however, cardiogenic shock induces renal dysfunction from both low stroke volume and congestion. To be more precise, I try to think of this as poor forward flow from cardiac dysfunction.
These patients need to have the underlying cause treated, and then consider RV, LV, supportive therapy with inotropes, inodilators, vasodilators etc.
This is a rare phenotype for most ward patients, but is something we encounter regularly in the ICU.
(8/x) Interested in thoughts, suggestions, or comments on this?
From medical educators involved in undergraduate education, is it time for a shift towards hemodynamic AKI instead of pre-renal?
@TChanMD @Brent_Thoma @katiewiskar @uOttawamwoo @IM_POCUS @CardioNerds
From medical educators involved in undergraduate education, is it time for a shift towards hemodynamic AKI instead of pre-renal?
@TChanMD @Brent_Thoma @katiewiskar @uOttawamwoo @IM_POCUS @CardioNerds
Loading suggestions...





![(4/x) Hypovolemic AKI (or even better, low mean systemic filling pressure [Pmsf]).
True hypovolemia...](https://pbs.twimg.com/media/Gc68taaWoAARFcd.png)