ICU Hemodynamics Secrets:
Actually, these are not secrets at all; they reflect common, basic knowledge. But the word “secrets” is more clickbait-y!
Here it begins:
1. You don’t have to check for fluid responsiveness (FR) if the patient is bleeding to death…
Actually, these are not secrets at all; they reflect common, basic knowledge. But the word “secrets” is more clickbait-y!
Here it begins:
1. You don’t have to check for fluid responsiveness (FR) if the patient is bleeding to death…
2. Preload challenges (eg, end-expiratory occlusion test or tidal volume challenge) are preferable to fluid challenges
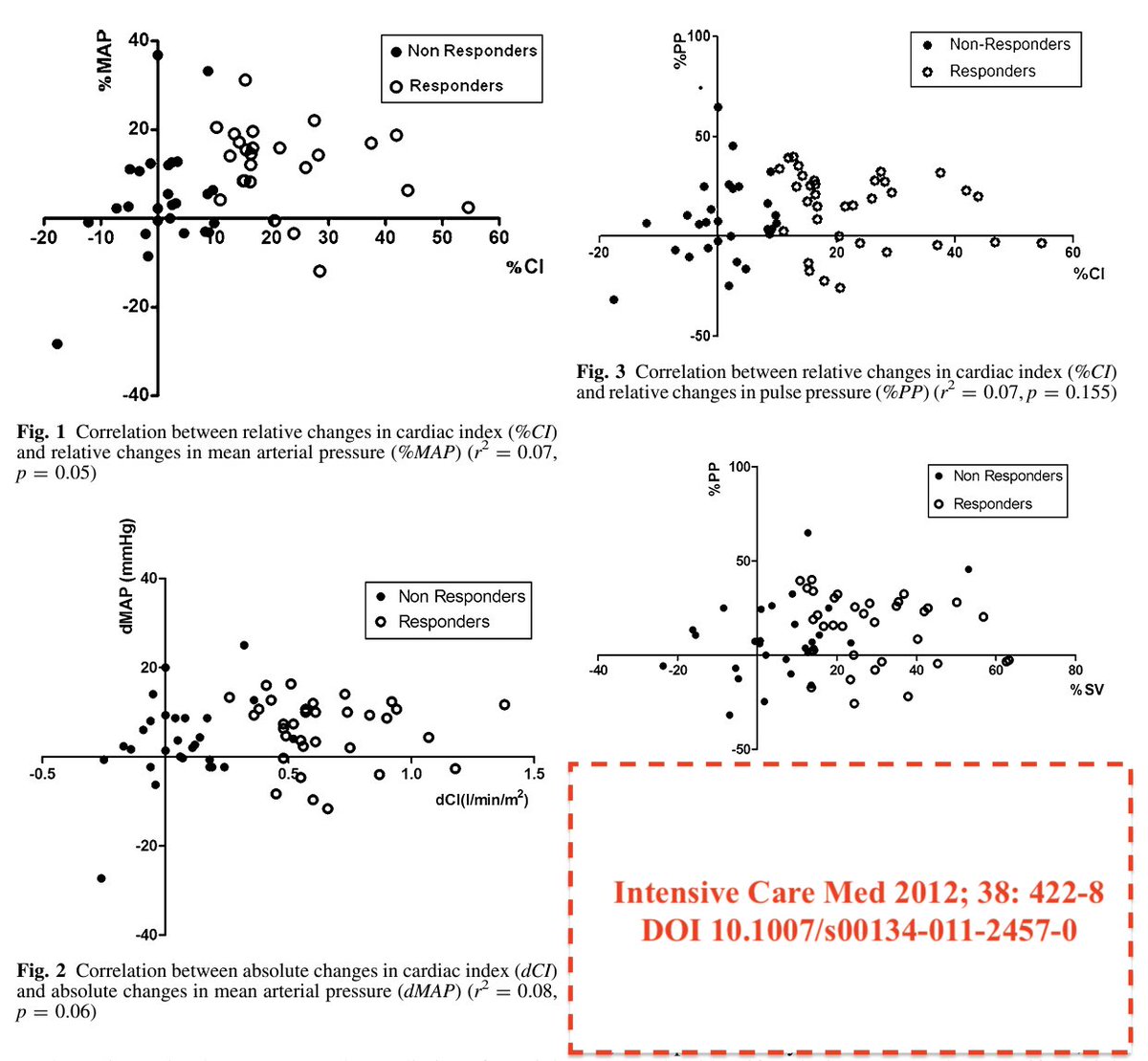
3. ~50% of pts do not respond to a fluid challenge (response defined as increase in cardiac output by >10%)
4. Even if the cardiac output ⬆️, this does not guarantee improvement in tissue oxygenation. In fact, only ~50% of those with CO ⬆️ will also show an ⬆️ in O2 consumption
4. Even if the cardiac output ⬆️, this does not guarantee improvement in tissue oxygenation. In fact, only ~50% of those with CO ⬆️ will also show an ⬆️ in O2 consumption
5. Please do the math by using the information in #3 and #4 👆
6. Fluid responsiveness is biventricular fluid responsiveness. The left ventricle cannot eject more blood than it receives from the right ventricle
The Frank-Starling curve and the Guyton's venous return curve cross each other in the right side of the heart!
The Frank-Starling curve and the Guyton's venous return curve cross each other in the right side of the heart!
9. CVP shouldn’t be used to predict FR, BUT it is not useless. For example, it is a warning signal for RV failure in a mechanically ventilated ARDS patient. And it is the downstream pressure for perfusion pressure; it is the “afterload” for liver and kidneys
10. Prone positioning is a hemodynamic intervention
Loading suggestions...