It is hard resuscitating patients on the ward 🏥
You don't have the same resources, personnel, or familiarity with the physical space. This can lead to slow and clunky resuscitations. 🦥
Here are 10 tips for smooth resuscitations on the ward that I learned as a paramedic (and now ICU doctor) 🚑
#medtwitter #foamed #foamcc
You don't have the same resources, personnel, or familiarity with the physical space. This can lead to slow and clunky resuscitations. 🦥
Here are 10 tips for smooth resuscitations on the ward that I learned as a paramedic (and now ICU doctor) 🚑
#medtwitter #foamed #foamcc
#1: Stay & Play vs. Scoop and Run
Borrowed from the pre-hospital world, some patients are best served with rapid transport to 'definitive care' and others benefit from more optimization on scene (ward) before transfer.
At my hospital, most patients in a non-monitored ward setting benefit from scoop and run to the ICU, with some exceptions. Eventually all these patients will be transferred to the ICU if critically ill, but the question is how much resus happens on the ward vs. ICU.
Scoop and Run
Massively bleeding patients (to OR if source known)
Known difficult airways needing semi-urgent intubation
Semi-urgent intubations in general
Stay and Play
Cardiac arrest (unless ECLS or some other therapy offered in ICU/OR)
Overdose / Decreased LOC not protecting airway (intubate so CT scans on way to ICU if needed)
Borrowed from the pre-hospital world, some patients are best served with rapid transport to 'definitive care' and others benefit from more optimization on scene (ward) before transfer.
At my hospital, most patients in a non-monitored ward setting benefit from scoop and run to the ICU, with some exceptions. Eventually all these patients will be transferred to the ICU if critically ill, but the question is how much resus happens on the ward vs. ICU.
Scoop and Run
Massively bleeding patients (to OR if source known)
Known difficult airways needing semi-urgent intubation
Semi-urgent intubations in general
Stay and Play
Cardiac arrest (unless ECLS or some other therapy offered in ICU/OR)
Overdose / Decreased LOC not protecting airway (intubate so CT scans on way to ICU if needed)
#2. Parallel vs. Sequential Resuscitation
One of the biggest advantages to a resuscitative unit is the ability for a high functioning team to accomplish multiple tasks at once (think F1 pit crew) 🏎️
This is the norm in the ED/ICU/OR. It is harder to achieve the same performance on the ward.
When resuscitating on the ward, try to initiate parallel tasks (often parallel with rapid transport to the ICU).
One of the biggest advantages to a resuscitative unit is the ability for a high functioning team to accomplish multiple tasks at once (think F1 pit crew) 🏎️
This is the norm in the ED/ICU/OR. It is harder to achieve the same performance on the ward.
When resuscitating on the ward, try to initiate parallel tasks (often parallel with rapid transport to the ICU).
#3. Don't underestimate the transport time
Even if you are only 2 floors up from the ICU, transporting a patient into the unit (including patient transfer, monitors, untangling lines) often takes 10+ minutes.
Factor in realistic transfer times into your decisions about stay and play vs. scoop and run.
Even if you are only 2 floors up from the ICU, transporting a patient into the unit (including patient transfer, monitors, untangling lines) often takes 10+ minutes.
Factor in realistic transfer times into your decisions about stay and play vs. scoop and run.
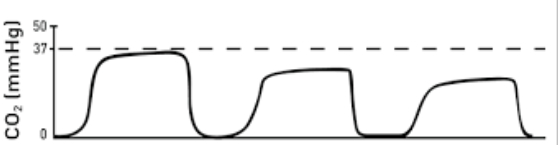
#4. Quantitative ETCO2 is the most powerful transport monitor
If you have quantitative capnography, monitor it during transport (especially in post arrest pts.)
If the ETCO2 it is 40mmHg then suddenly decreases to 30 and 25 the pt. is likely arresting (so long as you aren't overventilating)
This correlation with cardiac output is invaluable when other monitors (e.g. pulse ox / BP) may be inaccurate immediately post arrest.
If you have quantitative capnography, monitor it during transport (especially in post arrest pts.)
If the ETCO2 it is 40mmHg then suddenly decreases to 30 and 25 the pt. is likely arresting (so long as you aren't overventilating)
This correlation with cardiac output is invaluable when other monitors (e.g. pulse ox / BP) may be inaccurate immediately post arrest.
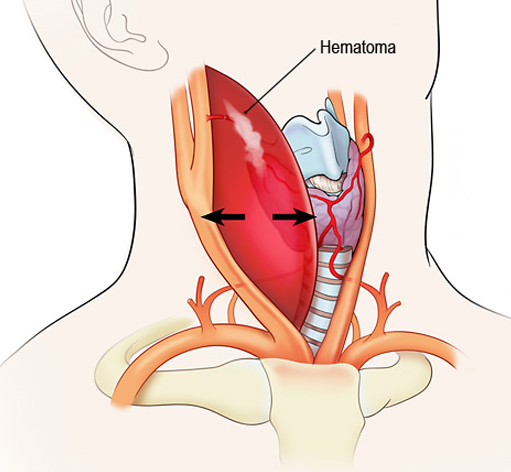
#5. Be wary of the evolving airway on the ward
(e.g. anaphylaxis or neck hematoma)
For patients with an evolving airway, despite their potential for difficulty with intubating, it may be necessary to secure the airway before transfer.
Call widely for help to get the appropriate backup (ENT, anesthesia, ICU etc.) as these can go south quickly.
(e.g. anaphylaxis or neck hematoma)
For patients with an evolving airway, despite their potential for difficulty with intubating, it may be necessary to secure the airway before transfer.
Call widely for help to get the appropriate backup (ENT, anesthesia, ICU etc.) as these can go south quickly.
#7: Don't be fancy
In a resuscitative environment feel free to get nuanced with resuscitation strategies. Your intubation meds can resemble a fancy NY cocktail 🍸
On the ward, keep it simple and use medications that are easily accessible, safe, and effective (my go to: Ketamine and Rocuronium for intubation)
For ventricular arrythmia, I love lidocaine as it is widely available and can be pushed safely.
In a resuscitative environment feel free to get nuanced with resuscitation strategies. Your intubation meds can resemble a fancy NY cocktail 🍸
On the ward, keep it simple and use medications that are easily accessible, safe, and effective (my go to: Ketamine and Rocuronium for intubation)
For ventricular arrythmia, I love lidocaine as it is widely available and can be pushed safely.
#8: Start Post Cardiac Arrest Patients on Vasopressors during transfer
If you achieve ROSC on a patient on the ward, even if their pressure is adequate, have pressors hooked up and ready to go.
Many of these patients will lose their BP 5-10 min later once the epinephrine circulating in their system wears off. Yes, pressors are safe peripherally during transport.
Often I will just start norepinephrine at 10mcg /min (~0.1mcg/kg/min) empirically for transport.
If you achieve ROSC on a patient on the ward, even if their pressure is adequate, have pressors hooked up and ready to go.
Many of these patients will lose their BP 5-10 min later once the epinephrine circulating in their system wears off. Yes, pressors are safe peripherally during transport.
Often I will just start norepinephrine at 10mcg /min (~0.1mcg/kg/min) empirically for transport.
#10: More is not always better
Running a code on the ward can be challenging because there are TOO many helpful hands.
My approach: instead of yelling 'I need everyone who isn't in this code to leave' and kicking people out of the room (which is confrontational and might result in new staff/learners missing out on crucial education), simply ask onlookers to be quiet. This accomplishes the same effect while being much less confrontational.
Running a code on the ward can be challenging because there are TOO many helpful hands.
My approach: instead of yelling 'I need everyone who isn't in this code to leave' and kicking people out of the room (which is confrontational and might result in new staff/learners missing out on crucial education), simply ask onlookers to be quiet. This accomplishes the same effect while being much less confrontational.
These are just a few tips and tricks! Would love to hear your best tricks for resuscitating patients on the ward.
#foamed #medtwitter #meded
#foamed #medtwitter #meded
جاري تحميل الاقتراحات...