1) Welcome to a 🆕#LIVE #accredited #tweetorial from #Basel 🇨🇭 & #ESOC2024, where we have just seen a new secondary analysis of #ANNEXa_I, the FIRST randomized comparison #andexanet_alfa vs usual care in pts with anti-#FXa #DOAC-associated #ICH. Another helping of data, please!
2) Our first-time expert author is #ANNEXa_I investigator David Seiffge MD @DavidSeiffge, Vascular neurologist at Inselspital Bern 🇨🇭
#FOAMed #FOAMcc #neurotwitter #cardiotwitter #ICH @ESOStroke @WorldStrokeOrg
#FOAMed #FOAMcc #neurotwitter #cardiotwitter #ICH @ESOStroke @WorldStrokeOrg
3) This program is supported by an independent educational grant from AstraZeneca. Statement of accreditation & faculty disclosures at cardiometabolic-ce.com. It is 🆓CE/#CME delivered wholly on Twitter for an audience of #healthcare providers!
#MedEd @MedTweetorials
#MedEd @MedTweetorials
4a) Remember when we brought you the #ANNEXa_I top-line results from #WSC23? Go back and (re)check that #tweetorial, and still earn more 🆓CE/#CME, at cardiometabolic-ce.com.
#MedEd @MedTweetorials
#ESOC2024
#MedEd @MedTweetorials
#ESOC2024
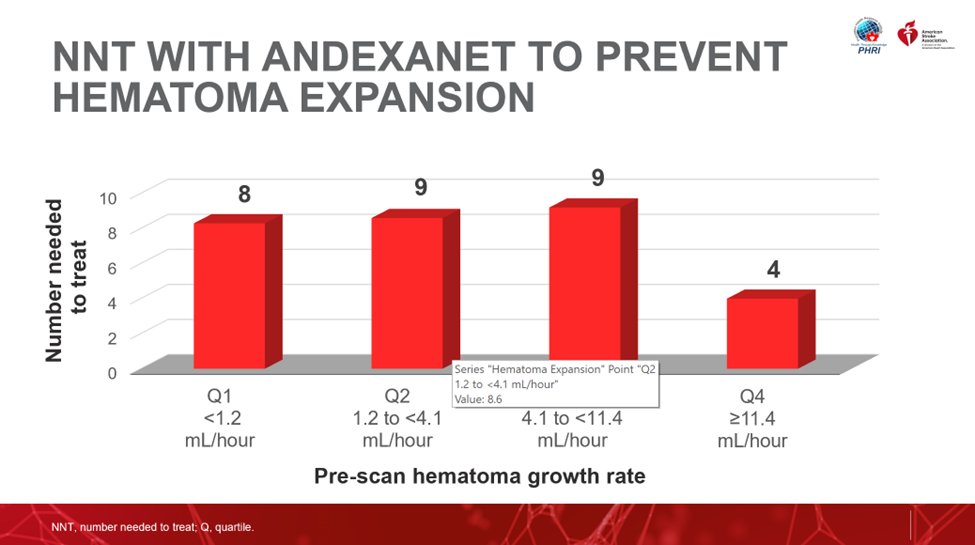
4b) We have subsequently kept you up to date on secondary analyses from that important trial. Again you can still earn CE/#CME by learning from @Ash_Shoamanesh about predictors of hematoma expansion in #ANNEXa_I patients: cardiometabolic-ce.com.
Now here we are at #ESOC2024.
Now here we are at #ESOC2024.
5c) Data from #ANNEXa_I are so important because despite that indication, pts with #DOAC-related #ICH are often treated with only support, or with nonspecific coagulation factor #repletion with an agent such as 4F-#PCC.
5d) As #ANNEXa_4 (🔓pubmed.ncbi.nlm.nih.gov), the trial that ➡️ authorization, was an open-label, single-cohort (#andexanet) study, a randomized study was needed to further explore its safety & efficacy. As there is no other approved tx, comparison was made to "usual care."
6b) Following a planned interim assessment of efficacy (n=450), an independent #DSMB concluded #andexanet showed superior hemostatic efficacy after 1mo f/u vs usual care, & stopped the trial early.
Hence the #LBCT at #WSC2023. Look for the full analysis to be published soon.
Hence the #LBCT at #WSC2023. Look for the full analysis to be published soon.
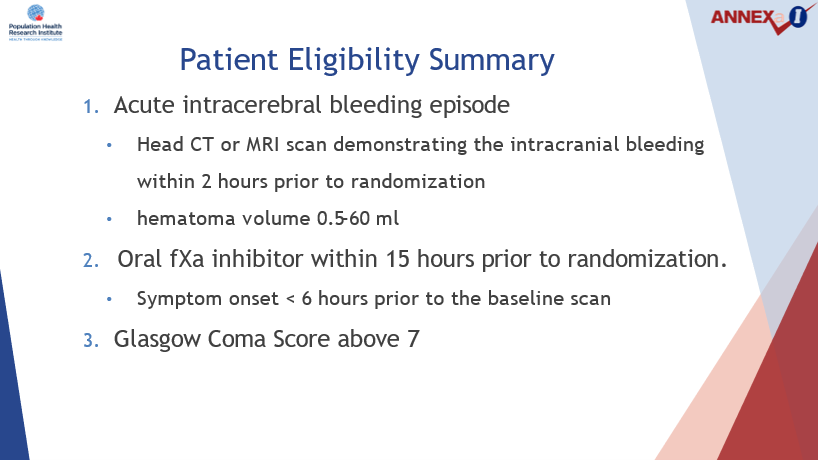
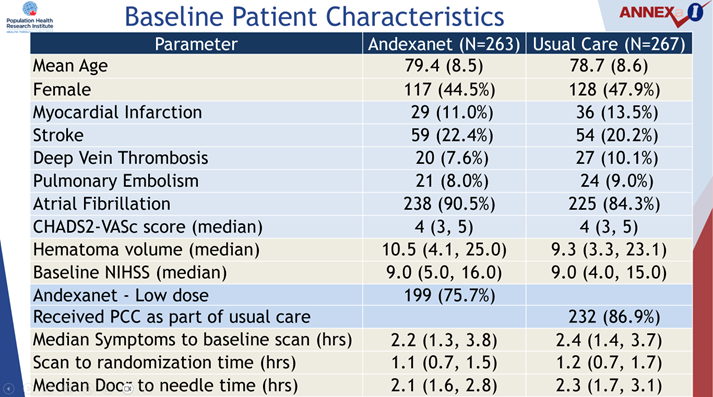
7) 530 participants were enrolled (263 assigned to #andexanet, 267 to usual care). Baseline characteristics appeared equally distributed between the two study arms. Mean age was ~79 years old; ~45% were ♀️ . Indication for OAC was #AF in 87%; median #CHA2DS2VASc score =4.
8b) Among those pts randomized to usual care, 87% received #PCC.
⏱️Mean symptoms ➡️ baseline scan = 2.3 hrs
⏱️Mean scan ➡️randomization = 1.2 hrs
⏱️Median door to 💉time in pts receiving #reversal or #repletion was 2.2 hrs
⏱️Mean symptoms ➡️ baseline scan = 2.3 hrs
⏱️Mean scan ➡️randomization = 1.2 hrs
⏱️Median door to 💉time in pts receiving #reversal or #repletion was 2.2 hrs
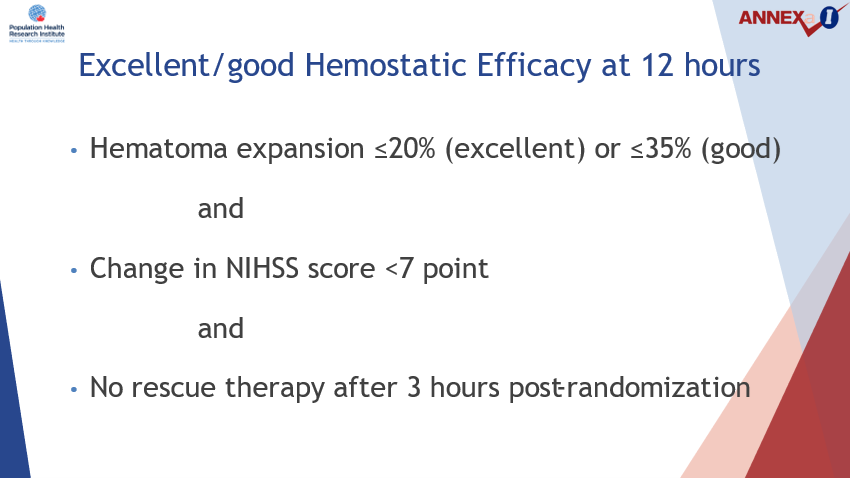
9) 🛑🩸Primary outcome: excellent or good #hemostatic efficacy occurred more often w/andexanet (64%) vs usual care (54%).
👉This ➡️11 more excellent/good #hemostatic efficacy outcomes /100 pts tx'd w/#andexanet.
👉Benefit driven mostly by ⬆️ rates of excellent hemostasis.
👉This ➡️11 more excellent/good #hemostatic efficacy outcomes /100 pts tx'd w/#andexanet.
👉Benefit driven mostly by ⬆️ rates of excellent hemostasis.
10) When using a higher threshold of #hematoma #expansion of 12.5 cc or more--which has a high #PPV for poor functional outcome in patients with #ICH at 90 days--there was a benefit 7 per 100 patients treated with #andexanet.
11) That “hematoma increase” of 12.5cc, or 35% expansion, was the focus of the first secondary analysis, which was presented by @Ash_Shoamanesh at #ISC24.
12) The objective of this pre-specified analysis was to identify patients participating in the #ANNEXa-I trial who were at greatest risk for hematoma expansion #HE & therefore were most likely to benefit from #andexanet
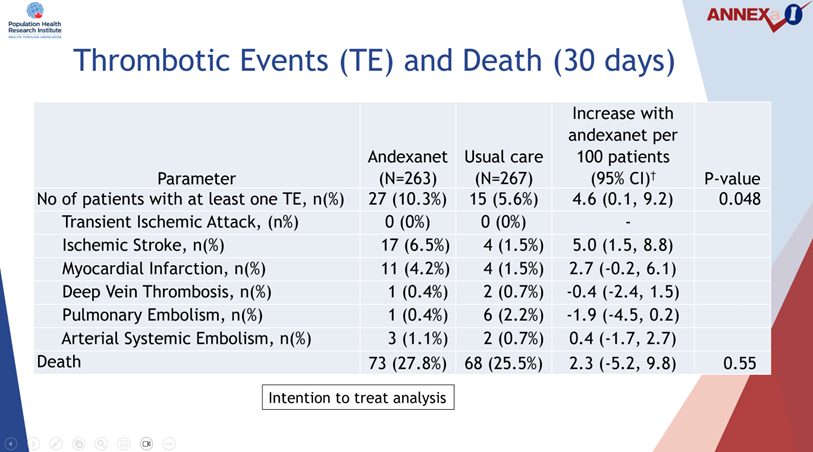
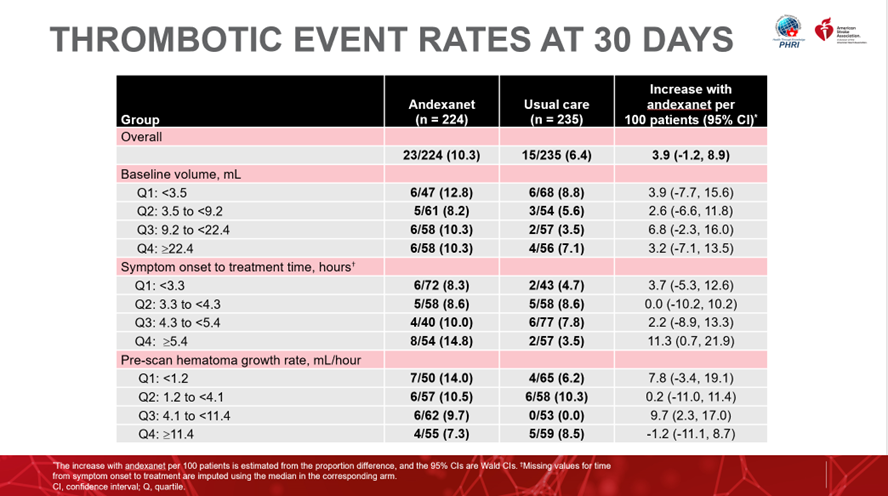
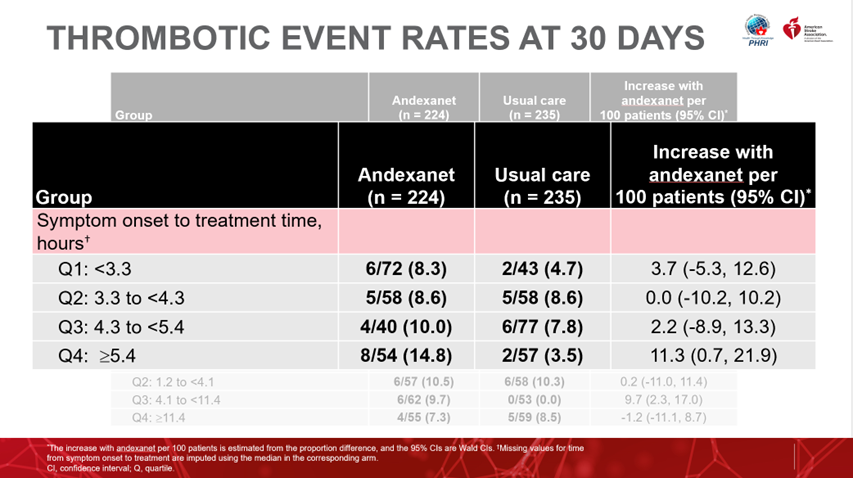
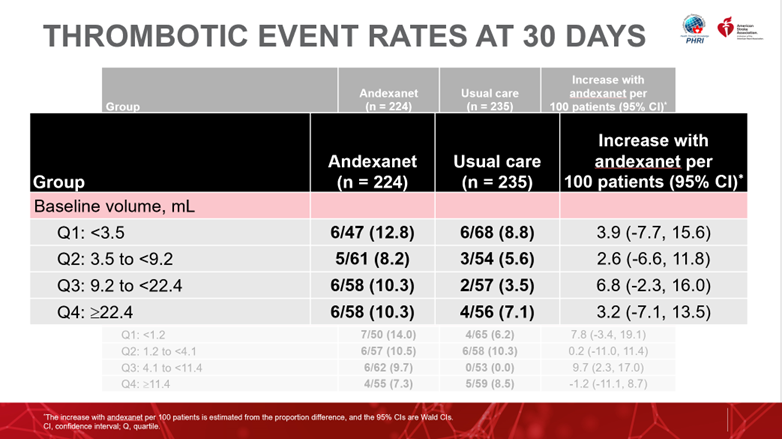
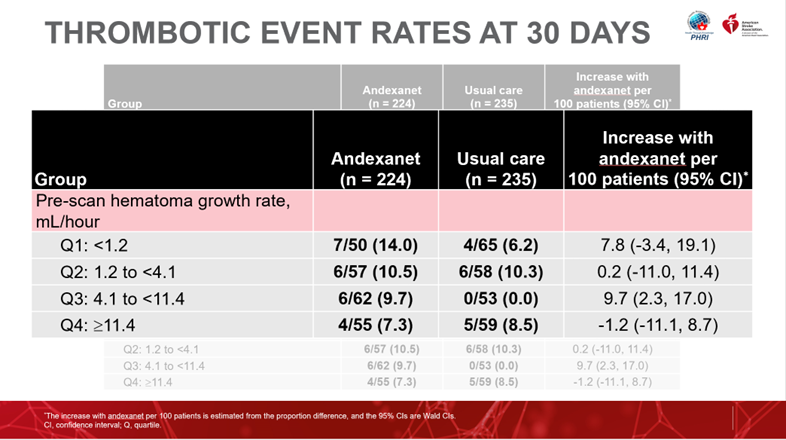
14a) Now you may also remember there was a higher rate of #thrombotic events seen with #andexanet (10%) vs usual care (6%) in #ANNEXa_I, ➡️ an ⬆️ of 5 pts with thrombotic events /100 pts treated with Andexanet, driven predominantly by a higher risk of ischemic #stroke.
15) Thus these metrics can be used to identify patients that would have the greatest benefit when balancing reduction in #hematoma expansion compared with potential excess #thrombotic events with #andexanet treatment.
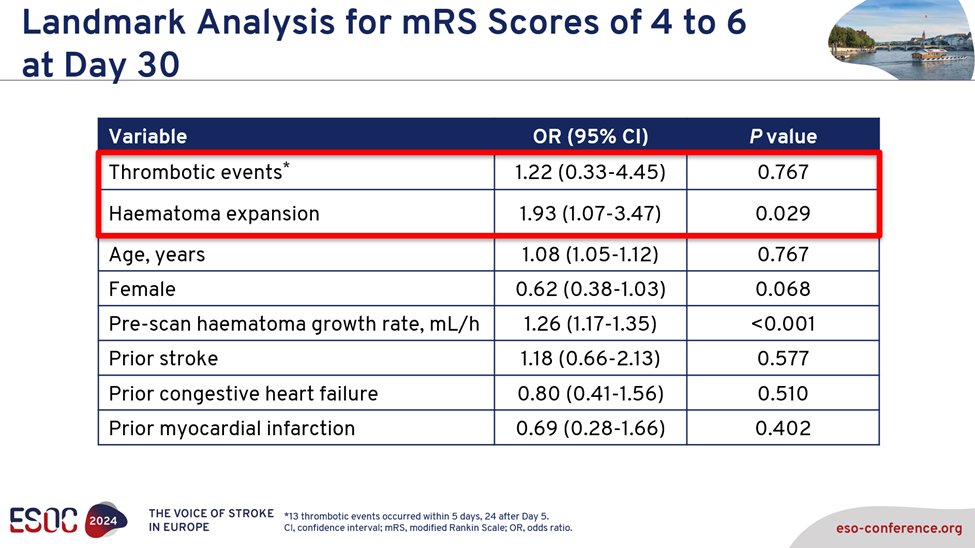
17) In this preplanned secondary analysis, #ANNEXa-I investigators sought to evaluate the clinical consequences of #HE and #thrombotic events (#TE) on all-cause mortality 🪦 and functional outcomes 🦽 to inform risk/benefit assessment of the use of #andexanet.
#ESOC2024
#ESOC2024
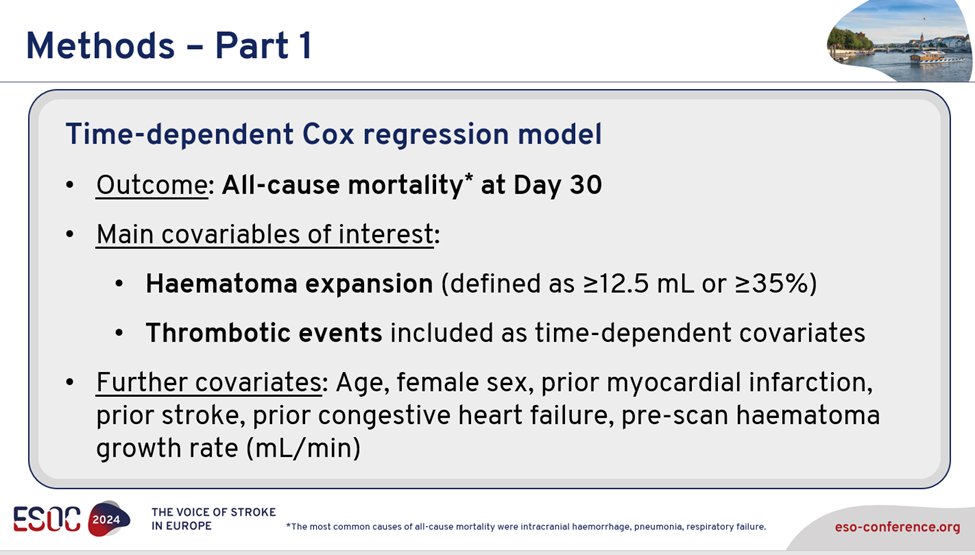
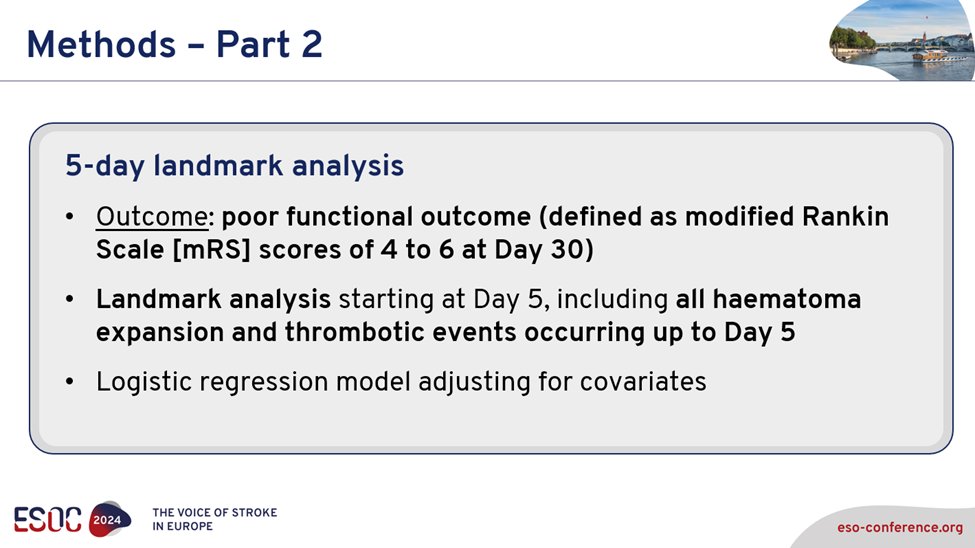
18a) The #methodology was robust: To assess the association with 30-day mortality, the authors used a #Cox_regression analysis including #HE along with other potential confounders. #TE were included as time-depending co-variable in this model.
18b) To assess the association with poor functional outcome at 30 days (defined as modified Rankin scale score #mRS 4-6), a landmark analysis approach was used, which included all #thrombotic events and #hematoma_expansion occurring until day 5 as baseline variables.
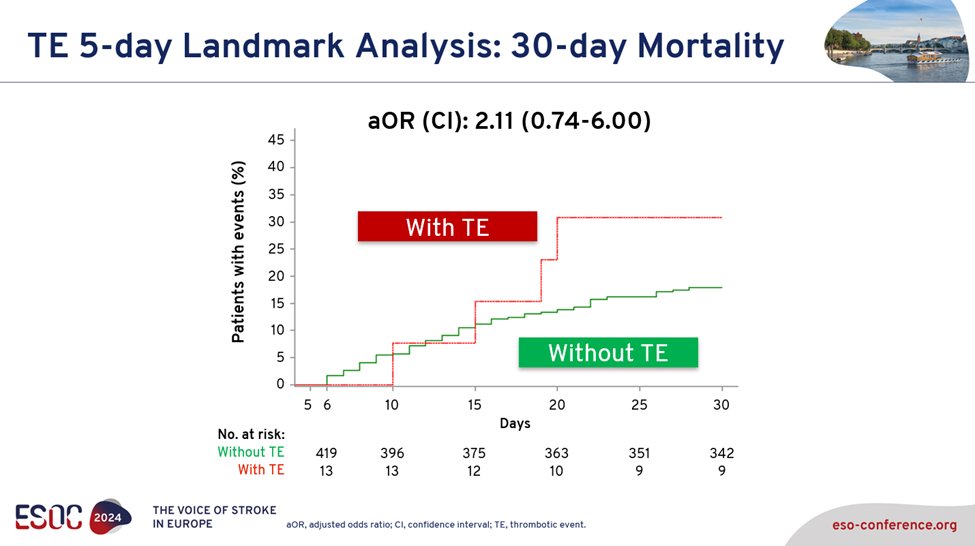
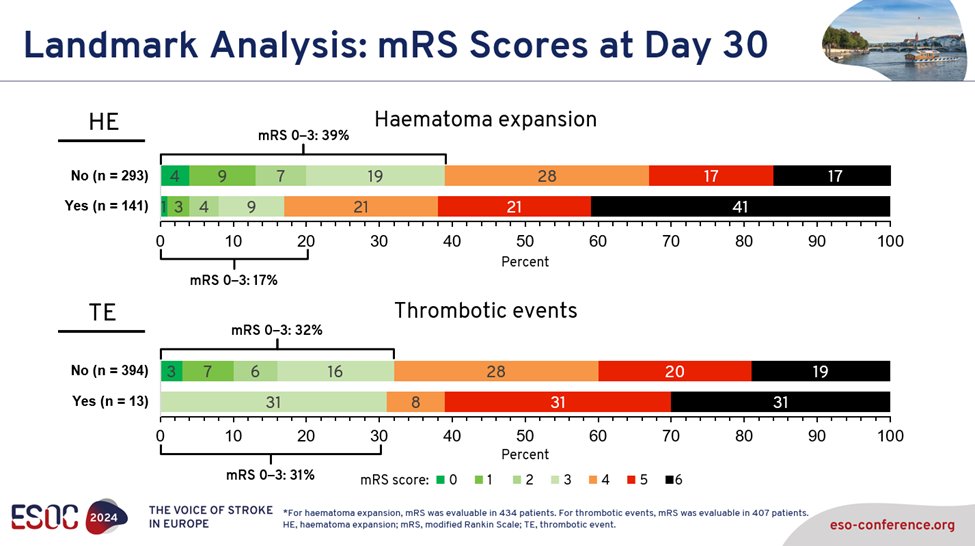
19) So what did they find? #Thrombotic events overall (particularly #arterial thrombosis) and #hematoma expansion both are strongly associated with 30d #mortality. Other potential predictors? Not so much.
20b) Note that due to the low event rate (only 13 #TE in the first 5 days), the Kaplan Meier curve is difficult to interpret.
20d) More important for many pts/next of kin is what happens to those pts who survive – what is their #functional outcome? That is why the authors also assessed the association w/poor outcome (mRS 4-6), i.e. this endpoint includes pts who are bedridden or in 🦽.
20f) Hey--who needs a reminder about #mRS?
4⃣ moderately severe disability; unable to walk or attend to bodily functions without assistance
5⃣ severe disability; bedridden, incontinent, requires continuous care
6⃣ expired, during the hospital stay or after d/c
4⃣ moderately severe disability; unable to walk or attend to bodily functions without assistance
5⃣ severe disability; bedridden, incontinent, requires continuous care
6⃣ expired, during the hospital stay or after d/c
21a) This analysis fills an important gap of knowledge: It clearly shows that haematoma expansion is deadly. #HE is also significantly associated with severe disability & poor outcome in survivors. Its prevention should be the first treatment 🎯.
21b) #Thrombotic events are also associated with #mortality, but their impact on poor functional outcome remains uncertain. It is important to realize that #HE is 4-times more frequent than #TE!
22) The #ESOC2024 presentation concluded:
23b) It's d, a & b. Interestingly, prior #stroke did not predict mortality. Now: which of these factors predicts poor #functional outcome at 30d?
a. TE
b. HE
c. age
d. prior stroke
a. TE
b. HE
c. age
d. prior stroke
25) .@DavidSeiffgecomments: Treating pts with FXaI #ICH is not simple – it is a ☠️disease in a high risk population. Our data should help clinicians make risk/benefit assessments. What is clear: #HE is frequent, deadly and those who survive have poor outcome.
#stopthebleeding
#stopthebleeding
26) Great job! It’s like you were right here in Basel!
Claim your 🆓 0.75hr CE/#CME NOW at cardiometabolic-ce.com.
Many thanks to @DavidSeiffge from #ESOC2024, who encourages YOU 🫵 to FOLLOW @cardiomet_ce for timely, engaging, expert-led #MedEd!
Claim your 🆓 0.75hr CE/#CME NOW at cardiometabolic-ce.com.
Many thanks to @DavidSeiffge from #ESOC2024, who encourages YOU 🫵 to FOLLOW @cardiomet_ce for timely, engaging, expert-led #MedEd!
جاري تحميل الاقتراحات...