1/12 - Mystery #1
You are seeing a patient recently diagnosed with heart failure and started on GDMT. You notice that their hemoglobin (HGB) has increased (12 → 13 g/dL) in the intervening weeks.
🤔Which medication is the likely cause of this increase in HGB?
You are seeing a patient recently diagnosed with heart failure and started on GDMT. You notice that their hemoglobin (HGB) has increased (12 → 13 g/dL) in the intervening weeks.
🤔Which medication is the likely cause of this increase in HGB?
2/12 - An Answer
Empagliflozin
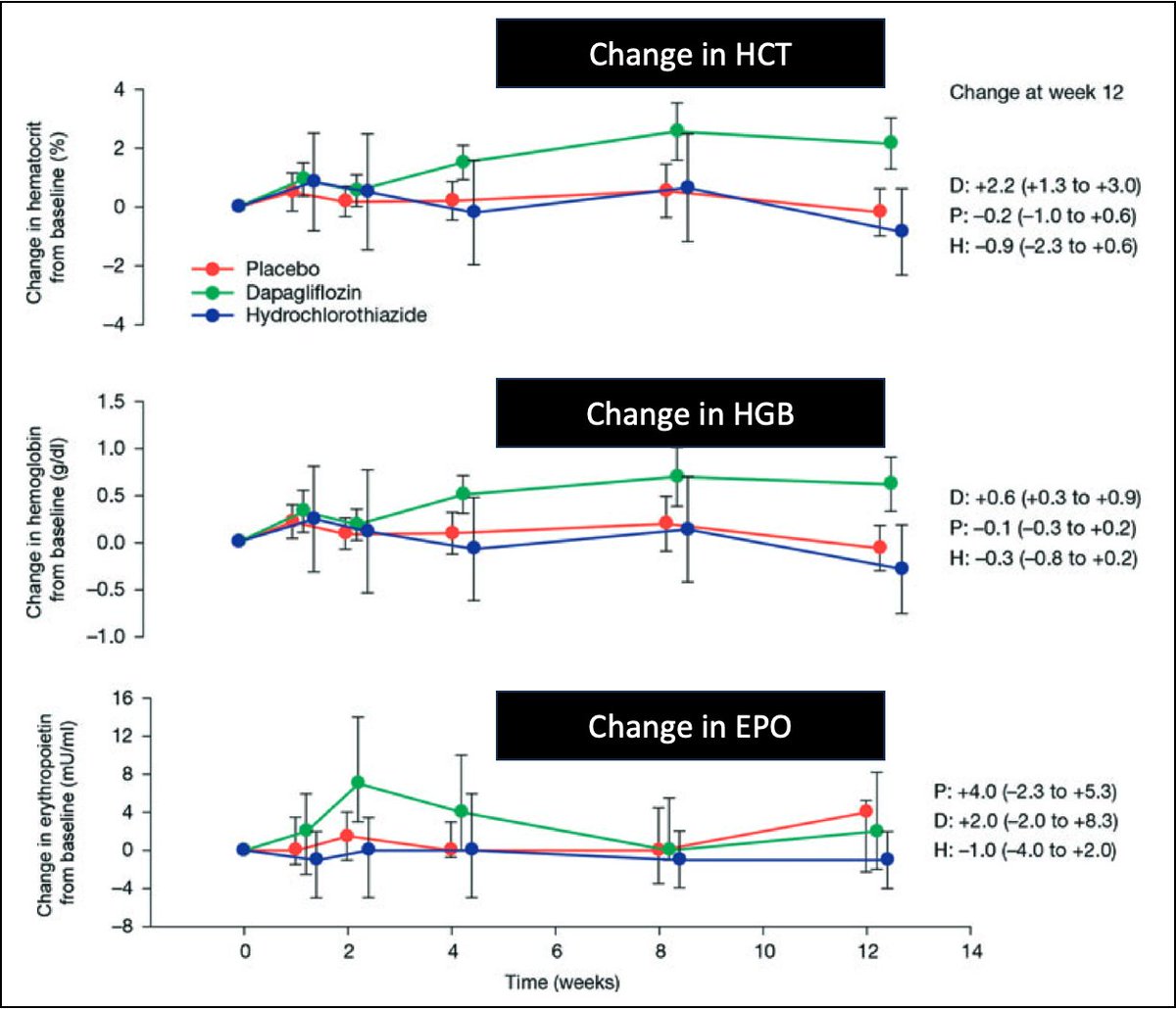
💡All SGLT2 inhibitors have been associated with an increase in hematocrit/hemoglobin soon after initiation.
The average increase is 2.3% in hematocrit and 0.6 g/dL in hemoglobin.
ncbi.nlm.nih.gov
Empagliflozin
💡All SGLT2 inhibitors have been associated with an increase in hematocrit/hemoglobin soon after initiation.
The average increase is 2.3% in hematocrit and 0.6 g/dL in hemoglobin.
ncbi.nlm.nih.gov
3/12 - An Initial Explanation (I)
The effect of SGLT2 inhibitors on HCT/HGB has been noted since the very first randomized control trial of dapagliflozin, published in 2010.
Initially, investigators assumed this was related to the diuretic effect of these drugs (i.e., a reduction in plasma volume led to an increase in HCT/HGB).
pubmed.ncbi.nlm.nih.gov
The effect of SGLT2 inhibitors on HCT/HGB has been noted since the very first randomized control trial of dapagliflozin, published in 2010.
Initially, investigators assumed this was related to the diuretic effect of these drugs (i.e., a reduction in plasma volume led to an increase in HCT/HGB).
pubmed.ncbi.nlm.nih.gov
4/12 - An Initial Explanation (II)
As more data accumulated, it became clear that a decrease in plasma volume alone could not explain the increase in HCT/HGB.
This is supported by the observation that diuretics like furosemide aren't typically associated with erythrocytosis.
pubmed.ncbi.nlm.nih.gov
As more data accumulated, it became clear that a decrease in plasma volume alone could not explain the increase in HCT/HGB.
This is supported by the observation that diuretics like furosemide aren't typically associated with erythrocytosis.
pubmed.ncbi.nlm.nih.gov
5/12 - An Alternative Explanation (I)
Some of the earliest studies of SGLT2 inhibitors noted an increase in red blood cell mass.
💡Alongside this was an increase in erythropoietin (EPO).
SGLT2 inhibitors seem to promote the generation of new red blood cells!
ncbi.nlm.nih.gov
Some of the earliest studies of SGLT2 inhibitors noted an increase in red blood cell mass.
💡Alongside this was an increase in erythropoietin (EPO).
SGLT2 inhibitors seem to promote the generation of new red blood cells!
ncbi.nlm.nih.gov
6/12 - An Alternative Explanation (II)
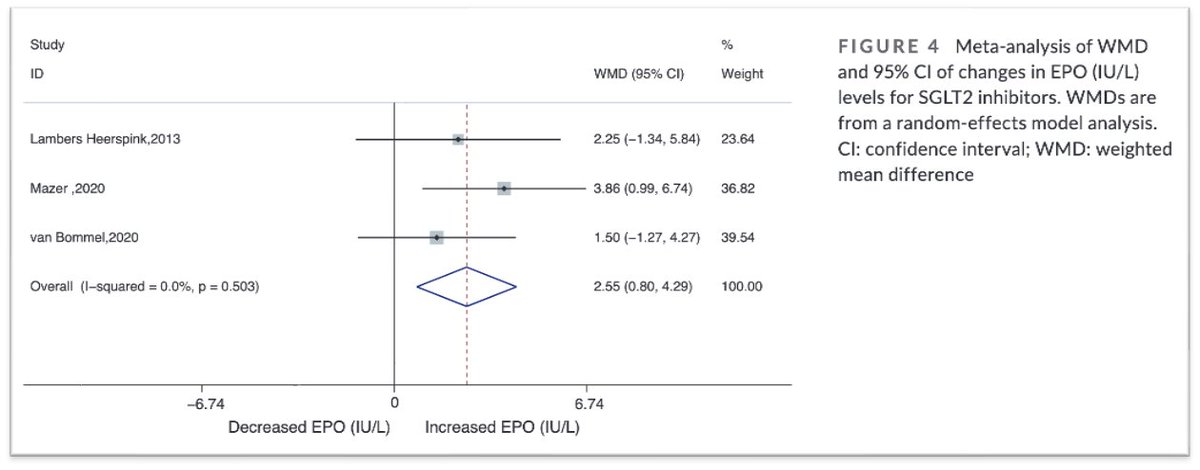
Subsequent data has confirmed this finding, with one meta-analysis suggesting a mean increase in EPO of about 2.55 IU/L.
ncbi.nlm.nih.gov
Subsequent data has confirmed this finding, with one meta-analysis suggesting a mean increase in EPO of about 2.55 IU/L.
ncbi.nlm.nih.gov
7/12 - Mystery #2
It now seems clear that SGLT2 inhibitors increase HCT/HGB via this increase in EPO.
The question becomes, why/how do they do that?
Taking a step back, one might ask: what organ is responsible for the increase in EPO?
It now seems clear that SGLT2 inhibitors increase HCT/HGB via this increase in EPO.
The question becomes, why/how do they do that?
Taking a step back, one might ask: what organ is responsible for the increase in EPO?
8/12 - An Answer (I)
A non-renal source of EPO is suggested by the observation that patients with CKD are still able to augment EPO production after starting an SGLT2 inhibitor.
If the anemia in CKD is, at least in part, related to a reduction in EPO production, this points to another source.
ncbi.nlm.nih.gov
A non-renal source of EPO is suggested by the observation that patients with CKD are still able to augment EPO production after starting an SGLT2 inhibitor.
If the anemia in CKD is, at least in part, related to a reduction in EPO production, this points to another source.
ncbi.nlm.nih.gov
9/12 - An Answer (II)
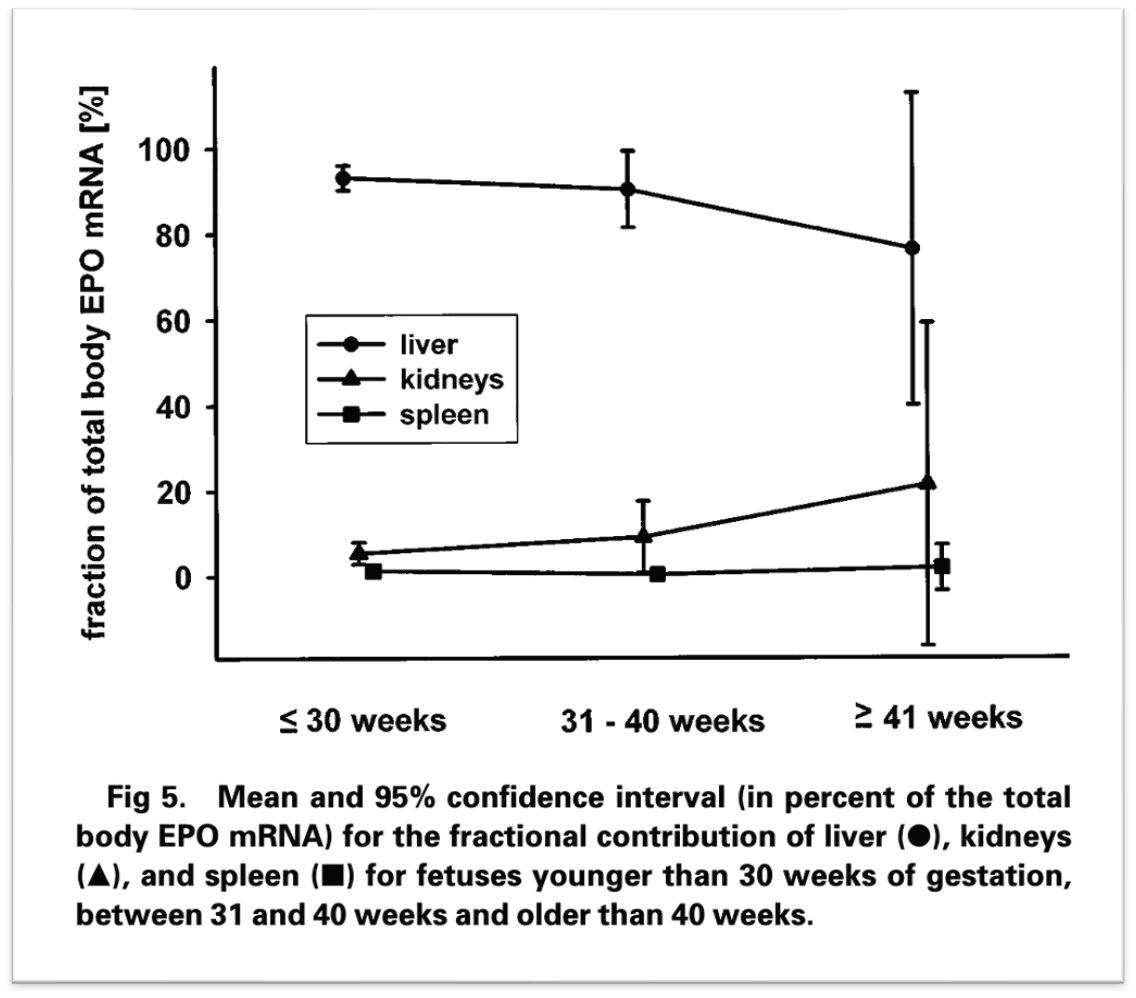
💡In utero, the liver is the main site of EPO production. After birth, this shifts to the kidney.
Does liver production of EPO ever kick back in for those with CKD?
pubmed.ncbi.nlm.nih.gov
💡In utero, the liver is the main site of EPO production. After birth, this shifts to the kidney.
Does liver production of EPO ever kick back in for those with CKD?
pubmed.ncbi.nlm.nih.gov
10/12 - An Answer (III)
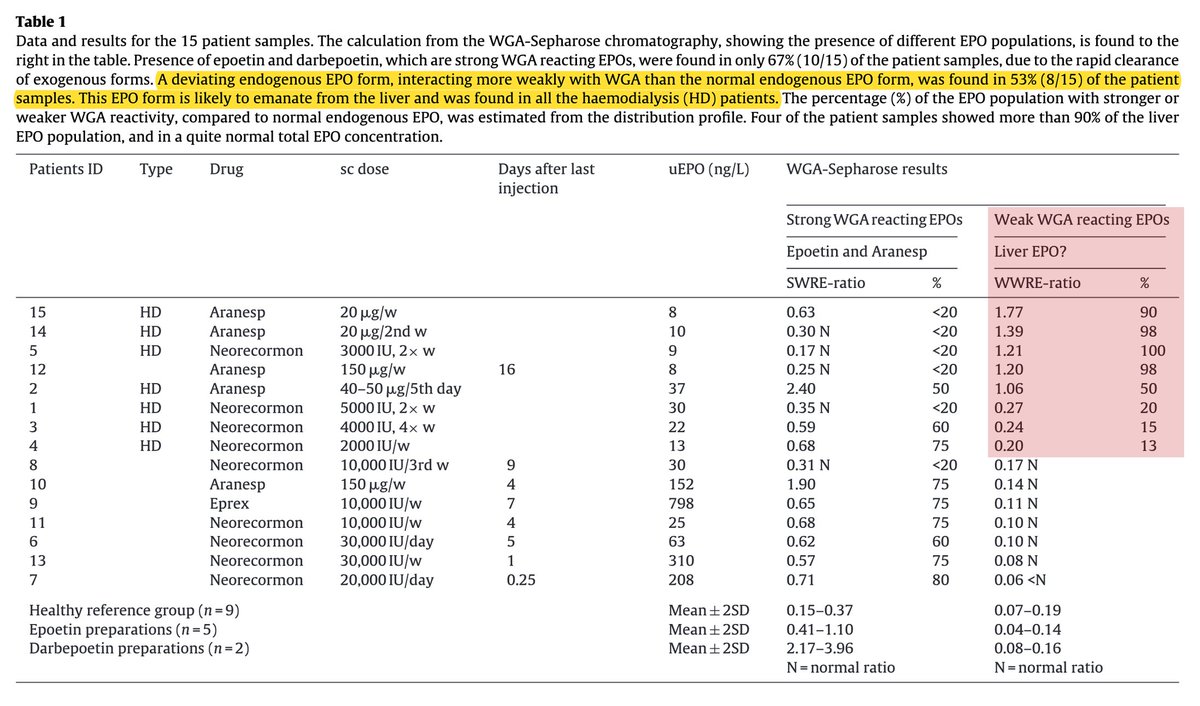
Some data suggest that liver production of EPO can increase in patients with ESRD.
In one study that included this population, 53% had evidence of liver EPO production.
In some cases, EPO levels rose back into the reference range! Notably, this still wasn't enough to correct the anemia.
pubmed.ncbi.nlm.nih.gov
Some data suggest that liver production of EPO can increase in patients with ESRD.
In one study that included this population, 53% had evidence of liver EPO production.
In some cases, EPO levels rose back into the reference range! Notably, this still wasn't enough to correct the anemia.
pubmed.ncbi.nlm.nih.gov
11/12 - An Explanation
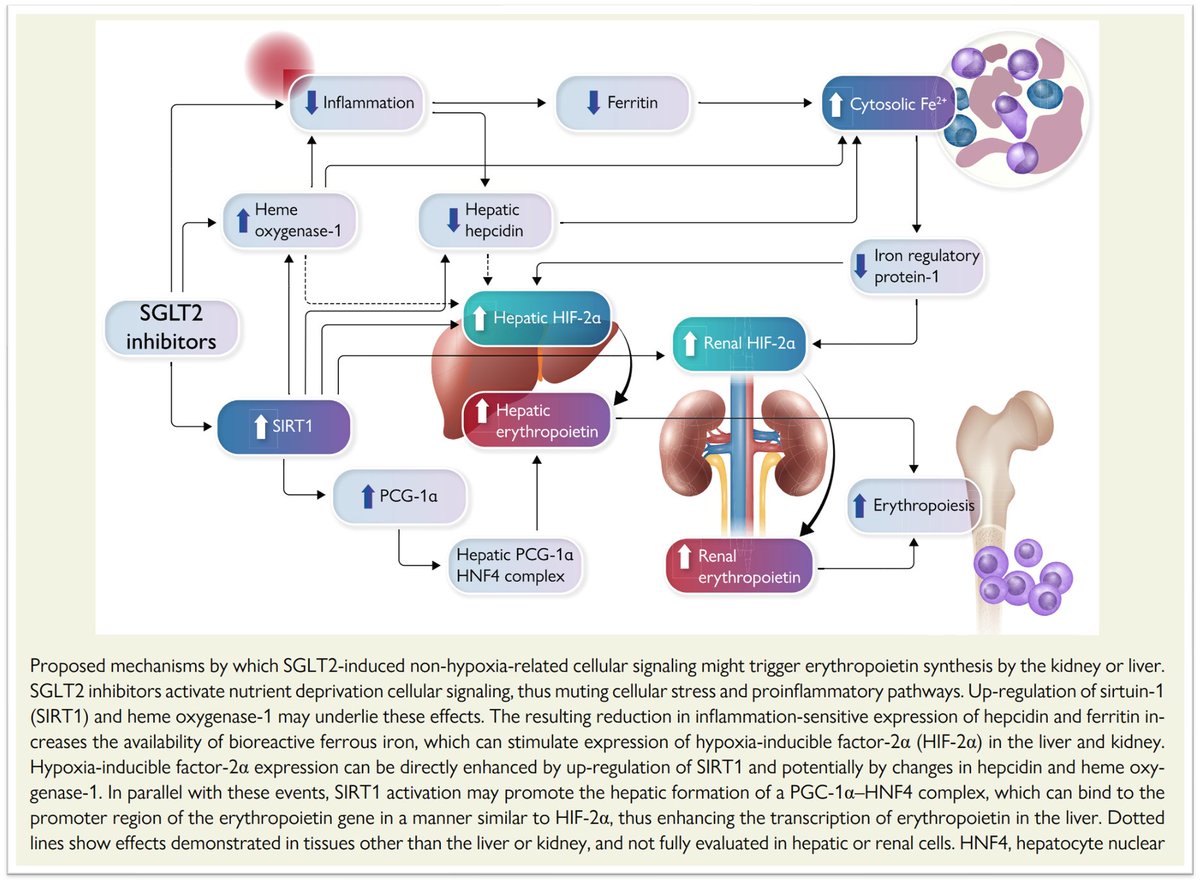
Milton Packer has suggested that SGLT2 inhibitors upregulate signaling pathways (via SIRT1, HIF-2α, and/or HNF4) to promote transcription of the erythropoietin gene in the liver.
It could be that these drugs turn on a quiescent liver function!
ncbi.nlm.nih.gov
Milton Packer has suggested that SGLT2 inhibitors upregulate signaling pathways (via SIRT1, HIF-2α, and/or HNF4) to promote transcription of the erythropoietin gene in the liver.
It could be that these drugs turn on a quiescent liver function!
ncbi.nlm.nih.gov
12/12 - Conclusion
There are likely additional pathways by which SGLT2 inhibitors augment kidney EPO production.
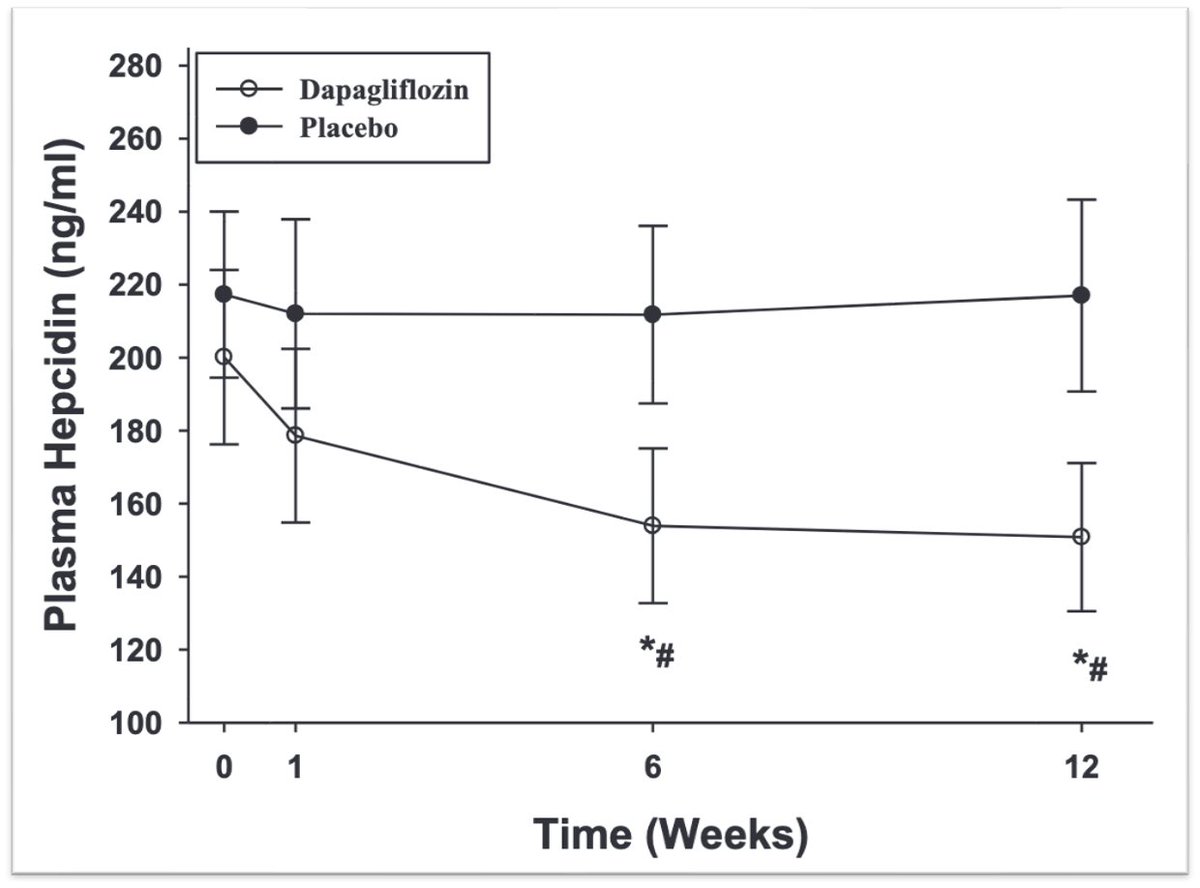
And there is fascinating data showing that these drugs decrease hepcidin, possibly mitigating some of the iron restriction seen in CKD and heart failure.
The myriad actions of SGLT2 inhibitors are fascinating!
pubmed.ncbi.nlm.nih.gov
There are likely additional pathways by which SGLT2 inhibitors augment kidney EPO production.
And there is fascinating data showing that these drugs decrease hepcidin, possibly mitigating some of the iron restriction seen in CKD and heart failure.
The myriad actions of SGLT2 inhibitors are fascinating!
pubmed.ncbi.nlm.nih.gov
Loading suggestions...