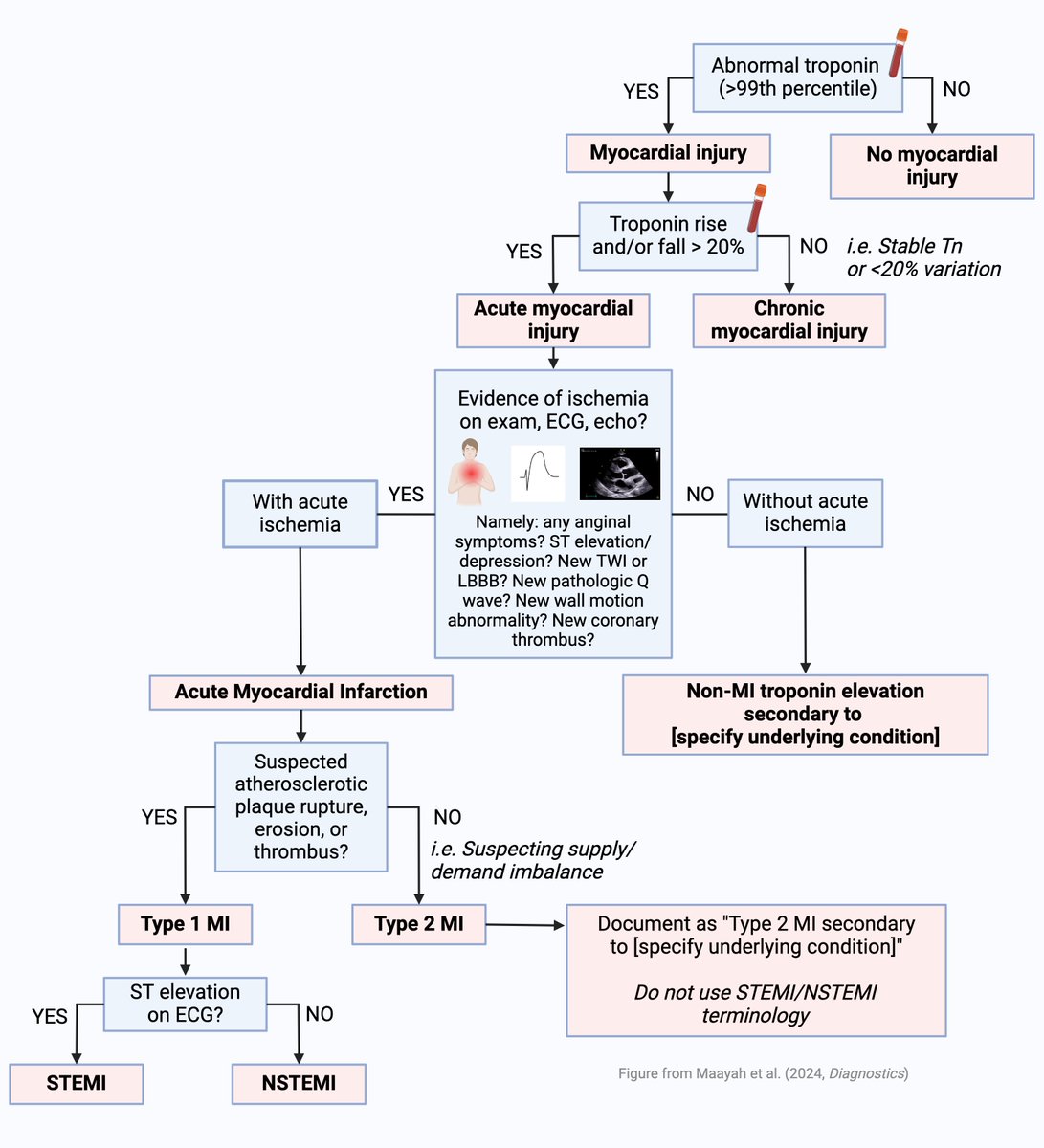
2⃣Is there a dynamic rise or fall in Tn, defined as >20% of the baseline Tn? If so, that is acute myocardial injury.
Is the Tn persistently elevated >99th %ile URL without a dynamic rise or fall? If so, that is chronic myocardial injury.
Is the Tn persistently elevated >99th %ile URL without a dynamic rise or fall? If so, that is chronic myocardial injury.
While there is enthusiasm for defining acute injury based on absolute “delta” changes in high-sensitivity Tn (hs-Tn) instead of the traditional 20%, research is ongoing to define the optimal delta threshold for each setting of care and manufacturer.
3⃣Is there any:
-Ischemic symptoms (e.g. exertional chest pain)?
-New ischemic ST/T/Q changes on ECG?
-New ischemic wall motion abnormalities on echo?
-New loss of viable myocardium on perfusion imaging?
-Evidence of a new coronary thrombus?
-Ischemic symptoms (e.g. exertional chest pain)?
-New ischemic ST/T/Q changes on ECG?
-New ischemic wall motion abnormalities on echo?
-New loss of viable myocardium on perfusion imaging?
-Evidence of a new coronary thrombus?
If so, that is acute myocardial ischemia.
If there are no ischemic ECG/echo changes and no ischemic symptoms, there is likely no myocardial ischemia. A diagnosis of non-MI Tn elevation due to [specify underlying cause] would be more appropriate.✅
If there are no ischemic ECG/echo changes and no ischemic symptoms, there is likely no myocardial ischemia. A diagnosis of non-MI Tn elevation due to [specify underlying cause] would be more appropriate.✅
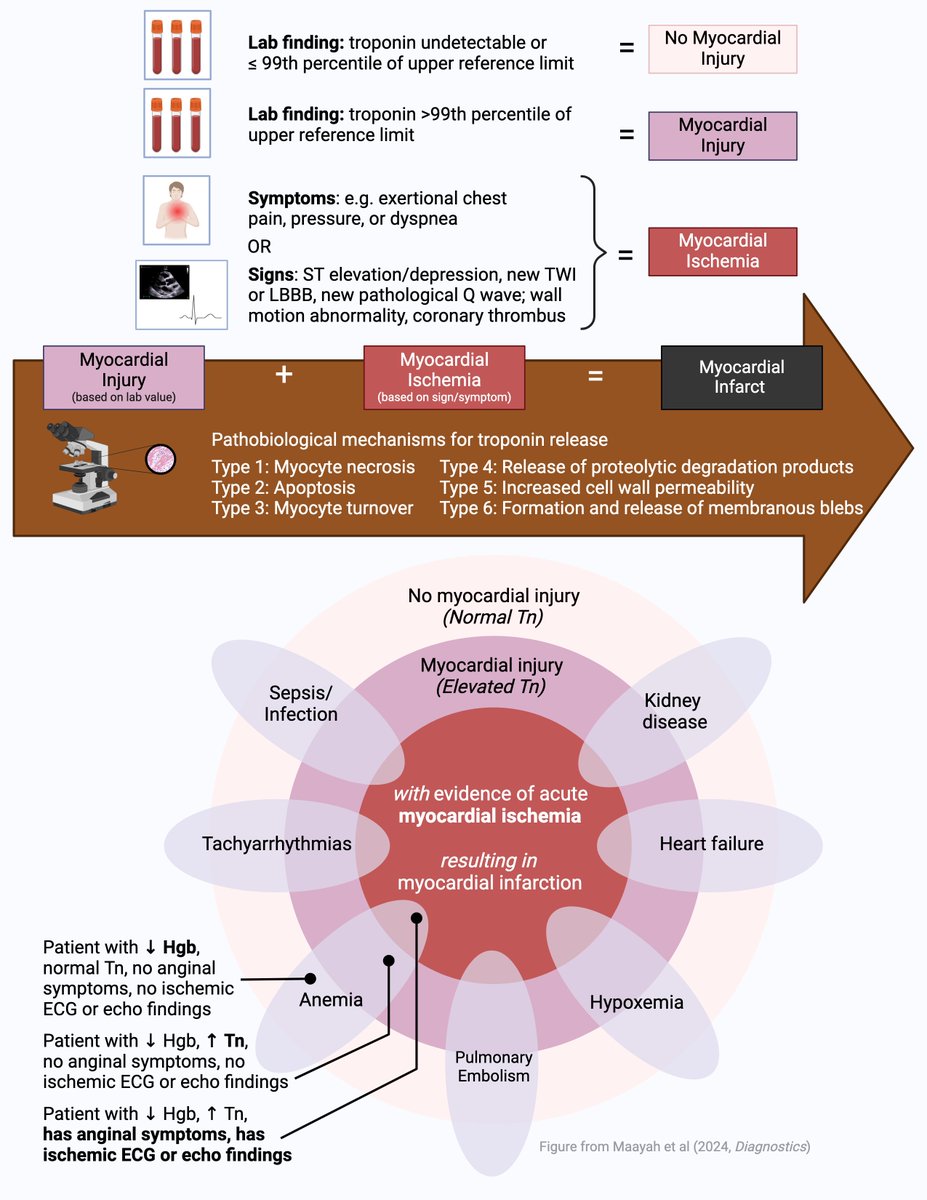
4⃣Myocardial infarction (MI) is defined by the presence of both acute myocardial injury and evidence of myocardial ischemia. Pathologically, MI is typically characterized by myocyte necrosis and/or apoptosis within hours.
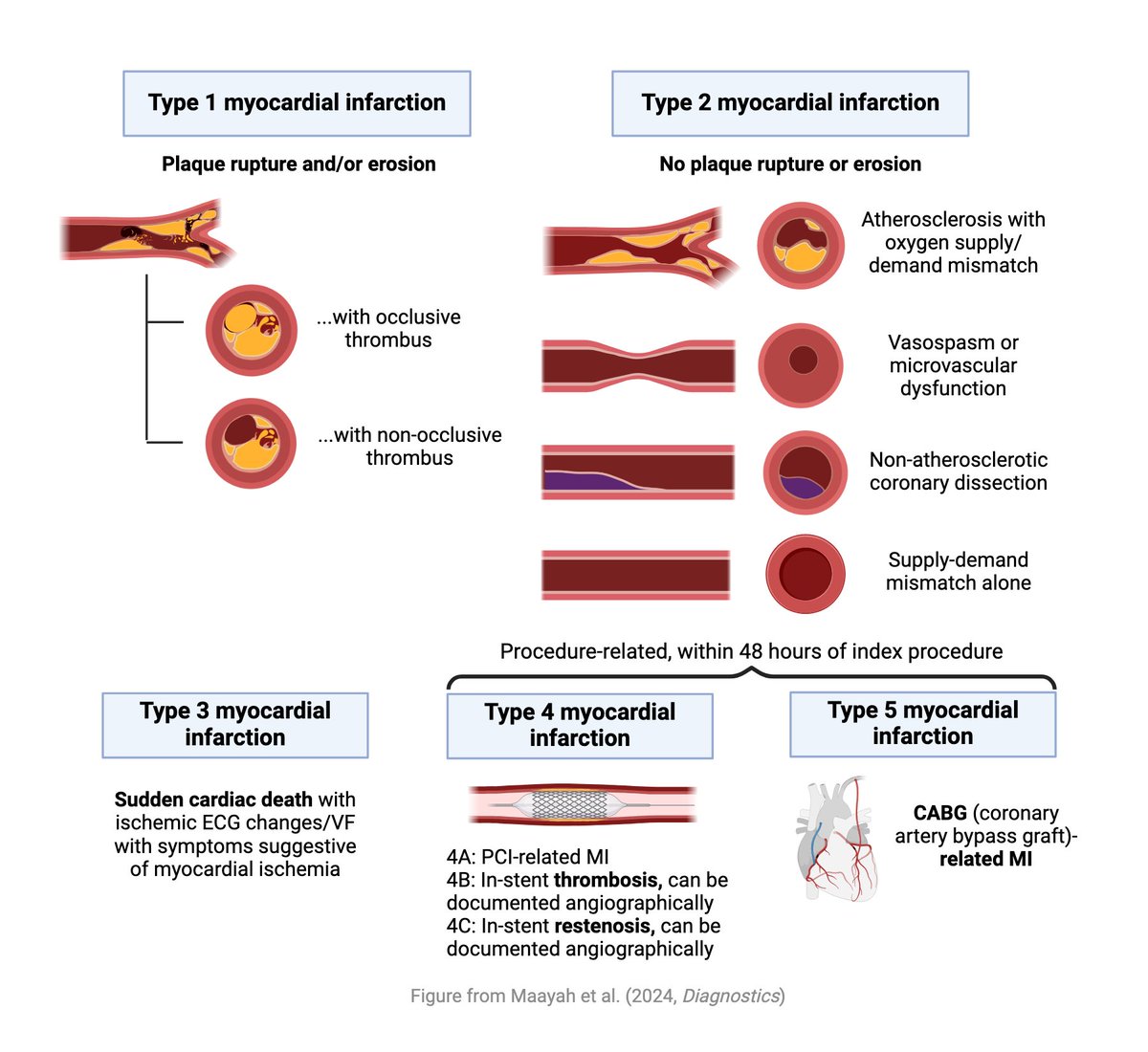
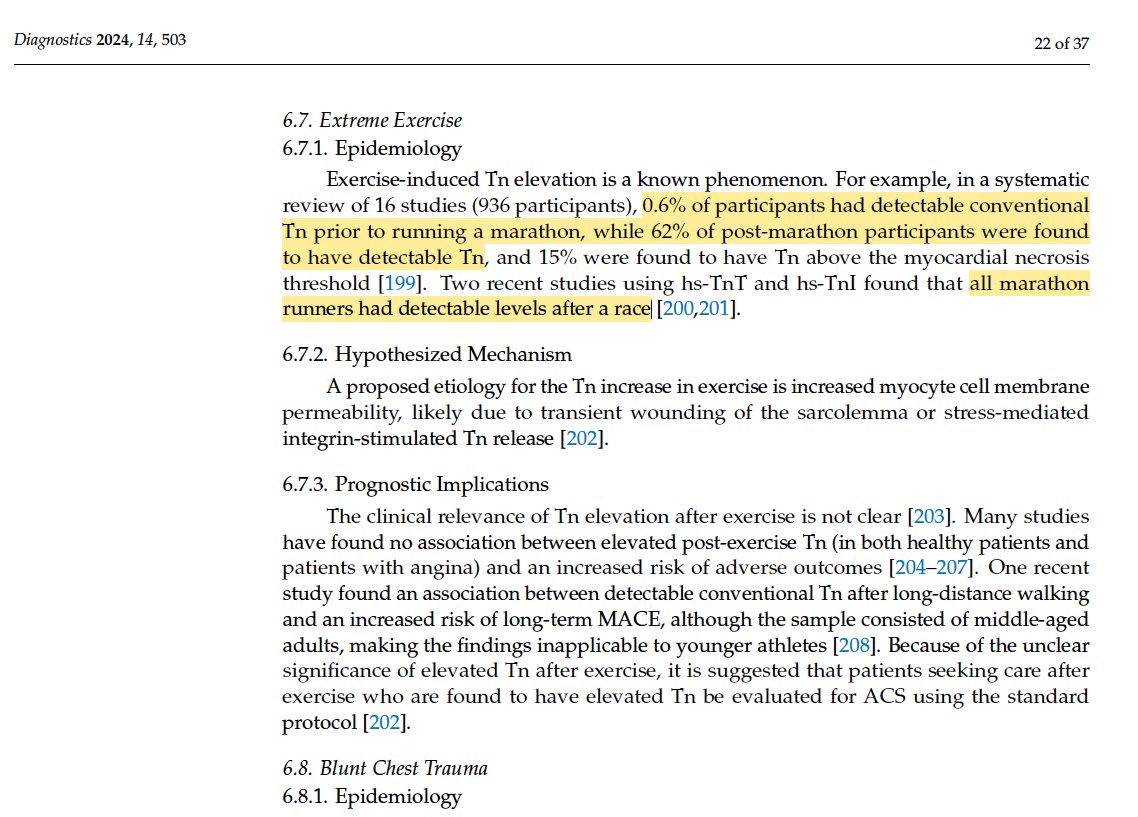
Type 2 MI can occur from increased oxygen demand alone, e.g. tachyarrhythmia, or from reduced oxygen delivery alone, e.g. severe anemia, hypoxemia, or bradyarrhythmia.
It is possible for supply-demand mismatch to occur on top of baseline atherosclerosis.
It is possible for supply-demand mismatch to occur on top of baseline atherosclerosis.
Type 2 MI can also occur from alternate processes such as vasospasm, microvascular dysfunction, or coronary artery dissection.
Type 3 MI refers to cases of sudden cardiac death with ischemic ECG changes (e.g. ventricular fibrillation) and/or symptoms suggestive of myocardial ischemia.
Type 4 MI refers to PCI-related MI.
Type 5 MI refers to CABG-related MI.
Type 4 MI refers to PCI-related MI.
Type 5 MI refers to CABG-related MI.
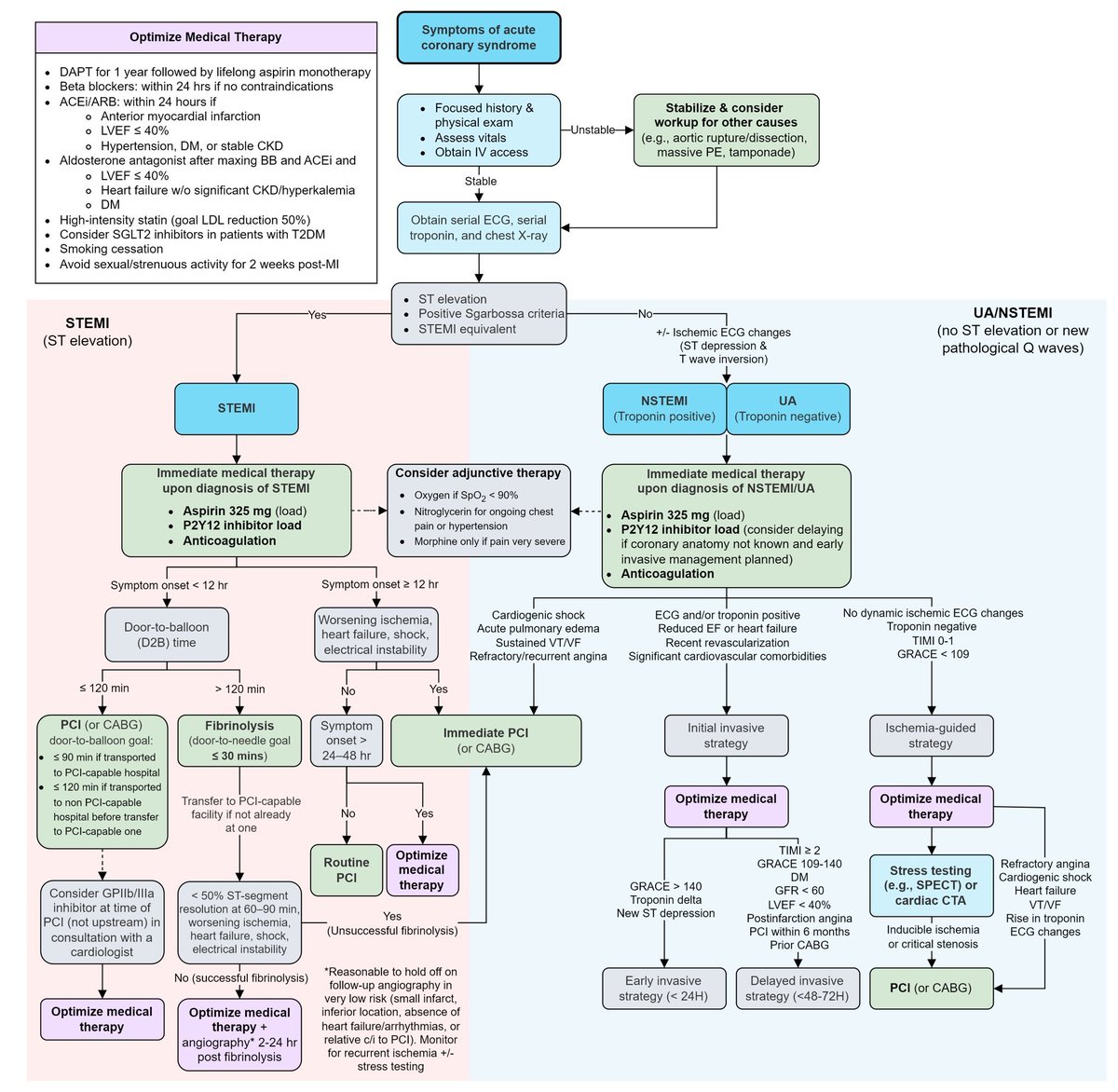
5⃣If there is ST elevation on ECG, the type 1 MI is a STEMI. All else falls under the umbrella of NSTE-ACS.
There is enthusiasm for ECG-based classification of type 1 MI as occlusive vs non-occlusive, but that has not yet made it to current guidelines.
There is enthusiasm for ECG-based classification of type 1 MI as occlusive vs non-occlusive, but that has not yet made it to current guidelines.
According to current guidelines, the terms “STEMI” and “NSTEMI” should only be used when referring to type 1 MI, not type 2 MI. “Type 2 NSTEMI” is a misnomer.❌
When you have a type 2 MI, document it as type 2 MI secondary to [specify underlying condition] ✅
For example, a patient with a drop in hemoglobin, normal Tn, and no anginal symptoms, ischemic ECG changes, or echo findings, has no myocardial injury.
A patient with a drop in hemoglobin, elevation in Tn, but no anginal symptoms, ischemic changes, or echo findings, has myocardial injury without myocardial ischemia.
Whereas a patient with a drop in hemoglobin, elevation in Tn, and either anginal symptoms, ischemic changes, or echo findings, has myocardial injury with myocardial ischemia, resulting in myocardial infarction.
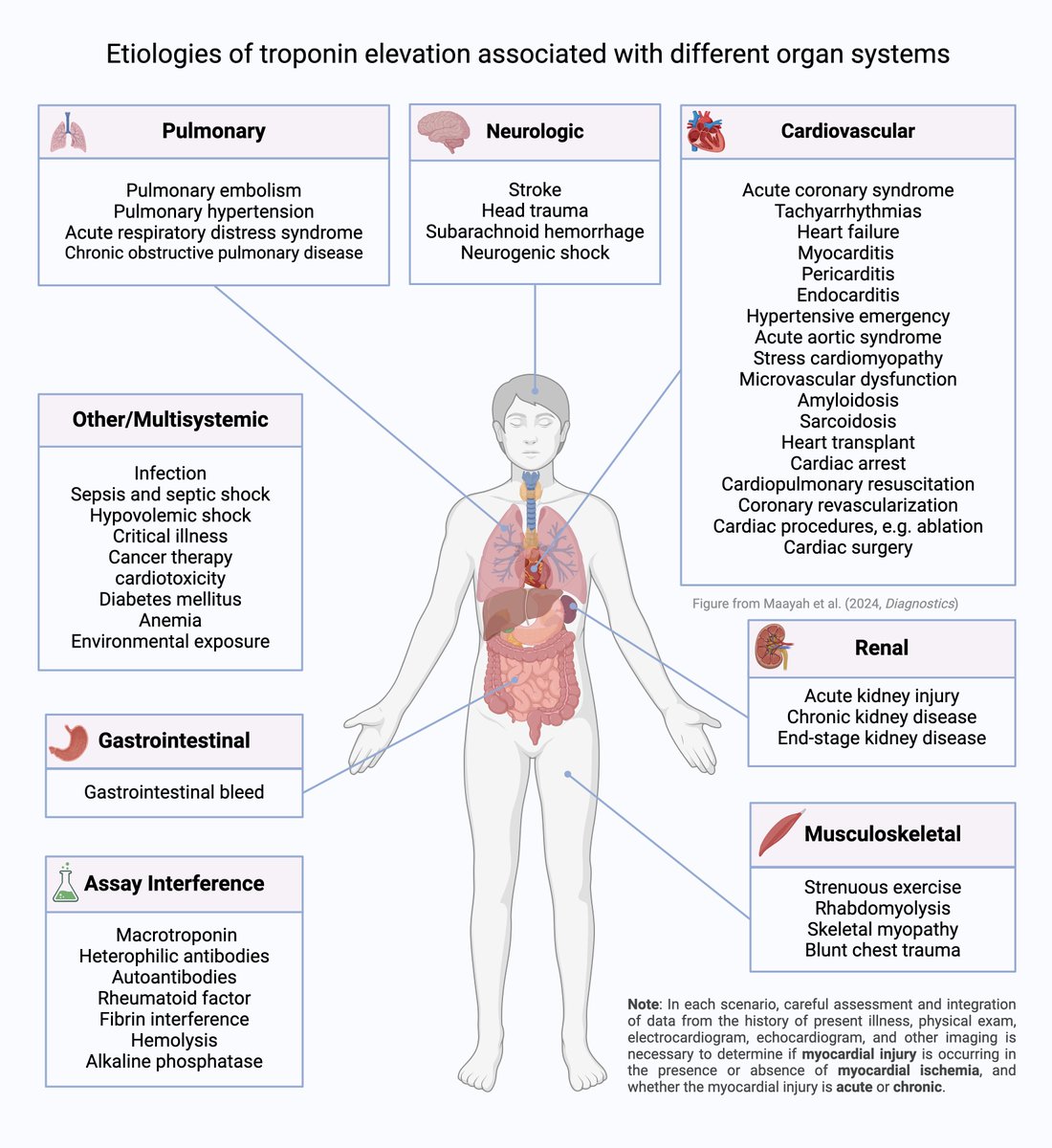
Check out this paper by Maayah @ScottGrubman Allen @ZacharyYeMed @daeyongp92 @evivemmou Gokhan @WSunMD Possick @jennkwanMDPhD Gandhi @ruey_hu from @YaleCardiology @YaleIMed @yaleem2 where these illustrations are from. doi.org
How would you rate the quality of this #tweetorial for your own learning and clinical practice?
Do you have any burning questions about interpretation of #troponin? Let us know, and we will add your questions (and answers) to troponin.org
While you're here, be sure to check out this thread from the Doctor of Documentation @Dr_Oubre reinforcing the importance of using correct troponin terminology
For a tweetorial focused on evidence-based diagnosis in ACS, check out my friend @SatyaPatelMD's summary:
@SatyaPatelMD For more of a focus on the management aspect, check out my friend @MatthewHoMD's trove of flowcharts.
@SatyaPatelMD @MatthewHoMD Also check out my buddy @ROKeefeMD's @pointofcaremed resource on ACS and MI: pointofcaremedicine.com
@SatyaPatelMD @MatthewHoMD @ROKeefeMD @pointofcaremed And this summary of the occlusive MI paradigm from EM thought leaders by @ASanchez_PS glass.health
@SatyaPatelMD @MatthewHoMD @ROKeefeMD @pointofcaremed @ASanchez_PS Since you've made it to this point, you deserve this clip about #tropomania from @DGlaucomflecken @cardiojaydoc02
Troponin figures are available in Portuguese courtesy of Dr Daniel Bandeira @dansbandeira @YaleCardiology
Troponin figures are available in Korean courtesy of Dr Dae Yong Park @YaleCardiology @CookCountyIMR
@YaleCardiology @CookCountyIMR Troponin figures are available in Arabic courtesy of Dr Ibrahim Alharbi @Dr_IbrahemSaleh
Loading suggestions...