1/
Have you ever been confused by prostatitis?
When to suspect it? How to diagnose it? How to treat it? Is it acute or chronic?
Read on for more information!
@sargsyanz @EvaAmenta @RizwanSohailMD @MelanieGoebelMD
Have you ever been confused by prostatitis?
When to suspect it? How to diagnose it? How to treat it? Is it acute or chronic?
Read on for more information!
@sargsyanz @EvaAmenta @RizwanSohailMD @MelanieGoebelMD
2/
Our comprehensive review of prostatitis is available here! 👇👇👇
pubmed.ncbi.nlm.nih.gov
It was a pleasure to work with @BCMIDFellowship fellow Tyler Brehm and @bwtrautner on this review!
Our comprehensive review of prostatitis is available here! 👇👇👇
pubmed.ncbi.nlm.nih.gov
It was a pleasure to work with @BCMIDFellowship fellow Tyler Brehm and @bwtrautner on this review!
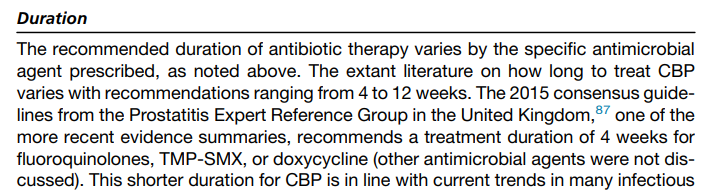
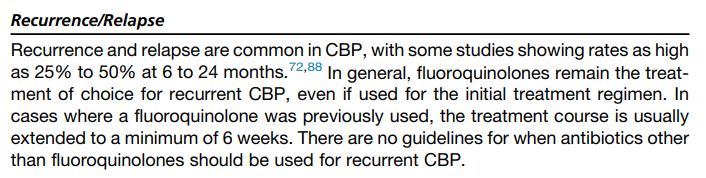
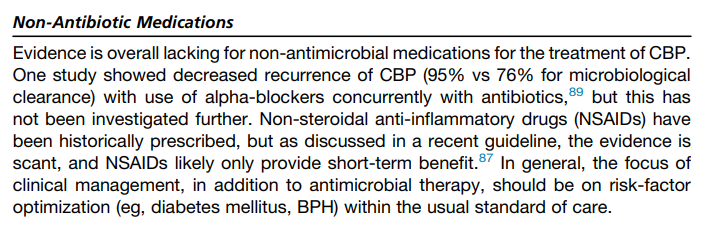
15/ Best options for treatment of chronic bacterial prostatitis??
Fluoroquinolones for 4-6 weeks
Trimethoprim-sulfamethoxazole for 6 weeks
Could *consider*:
Tetracyclines (doxycycline or minocycline)
Fosfomycin
Fluoroquinolones for 4-6 weeks
Trimethoprim-sulfamethoxazole for 6 weeks
Could *consider*:
Tetracyclines (doxycycline or minocycline)
Fosfomycin
19/ Summary!
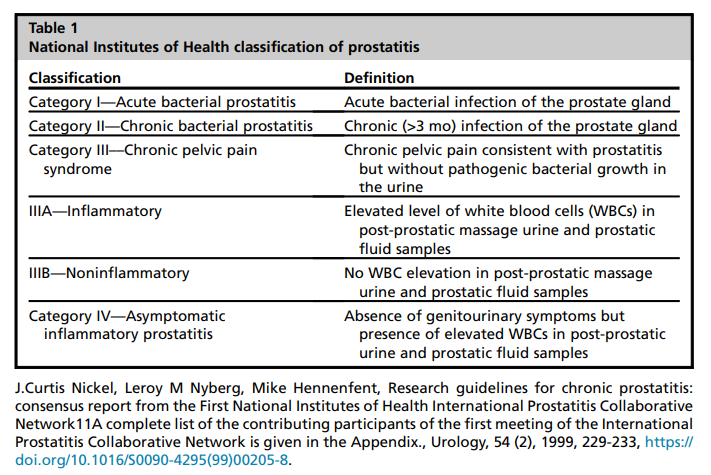
- Acute and chronic bacterial prostatitis are different entities.
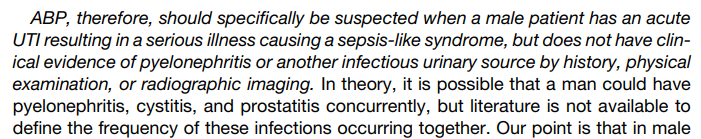
- Suspect ABP with sepsis of suspected urinary source and no evidence of pyelo or another urinary focus.
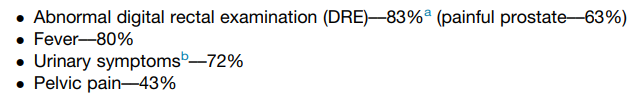
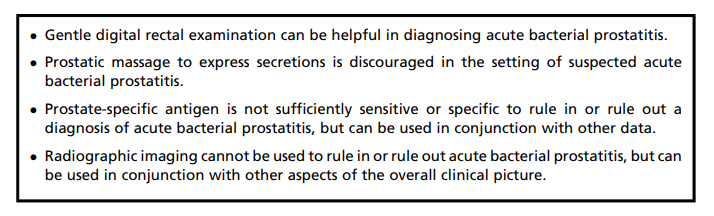
- ABP can be Dx'ed by clinical presentation and gentle DRE. Elevated PSA can support the Dx.
- Acute and chronic bacterial prostatitis are different entities.
- Suspect ABP with sepsis of suspected urinary source and no evidence of pyelo or another urinary focus.
- ABP can be Dx'ed by clinical presentation and gentle DRE. Elevated PSA can support the Dx.
20/ Summary! (continued)
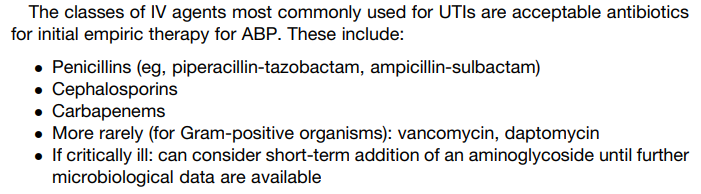
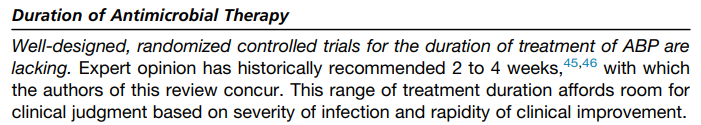
- ABP is treated with 2-4 weeks of Abx!
- CBP is indolent and should be suspected when a patient has recurrent UTIs due to the same organism.
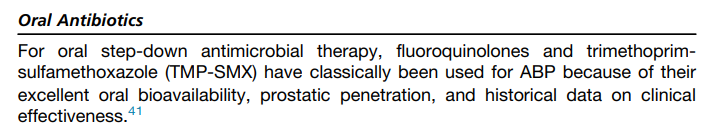
- Fluoroquinolones and TMP/SMX are best options for susceptible organisms with Rx of 4-6 weeks!
/End
- ABP is treated with 2-4 weeks of Abx!
- CBP is indolent and should be suspected when a patient has recurrent UTIs due to the same organism.
- Fluoroquinolones and TMP/SMX are best options for susceptible organisms with Rx of 4-6 weeks!
/End
Loading suggestions...