2/
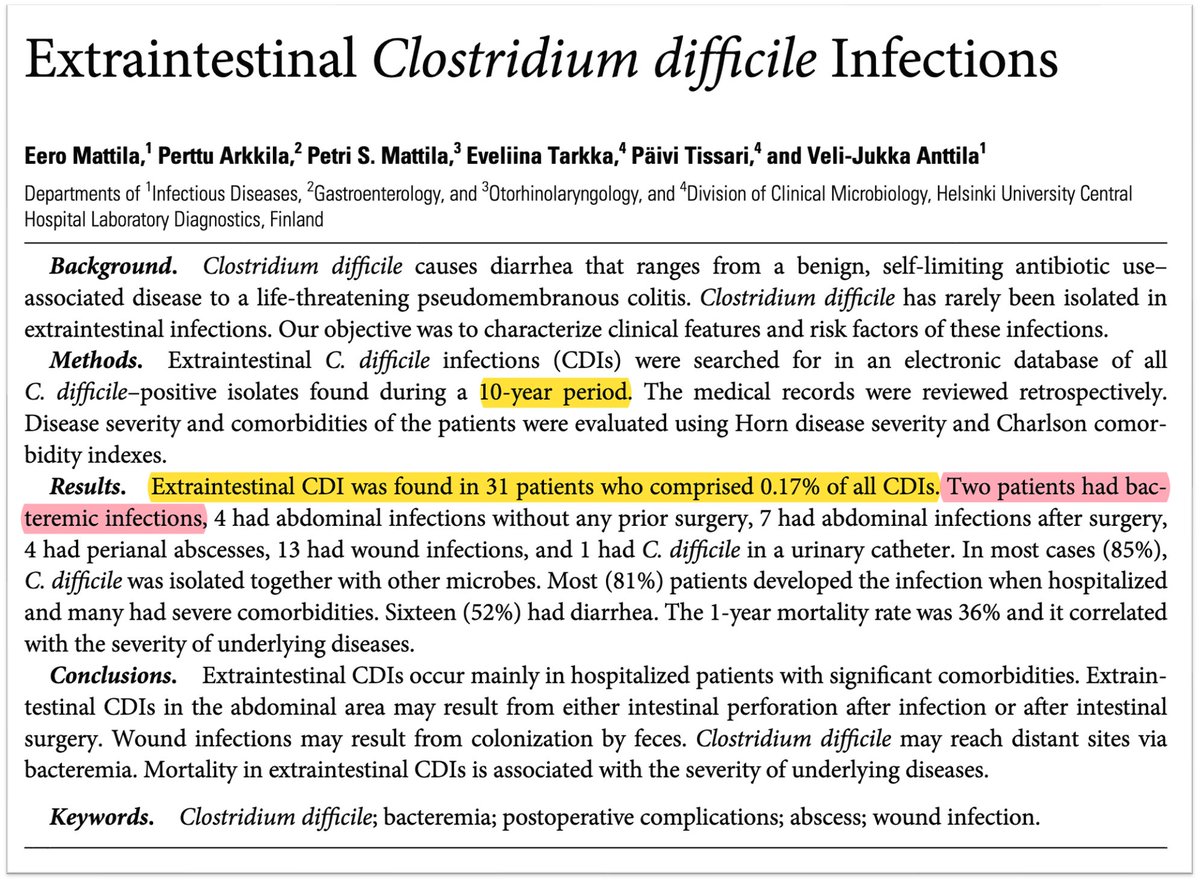
Extraintestinal manifestations of CDI are rare, in general.
One study examined a 10-year study and found that just 31 of 18,570 (0.17%) cases of CDI were extraintestinal.
💡And only 2 (0.01%) were bloodstream infections!
pubmed.ncbi.nlm.nih.gov
Extraintestinal manifestations of CDI are rare, in general.
One study examined a 10-year study and found that just 31 of 18,570 (0.17%) cases of CDI were extraintestinal.
💡And only 2 (0.01%) were bloodstream infections!
pubmed.ncbi.nlm.nih.gov
3/
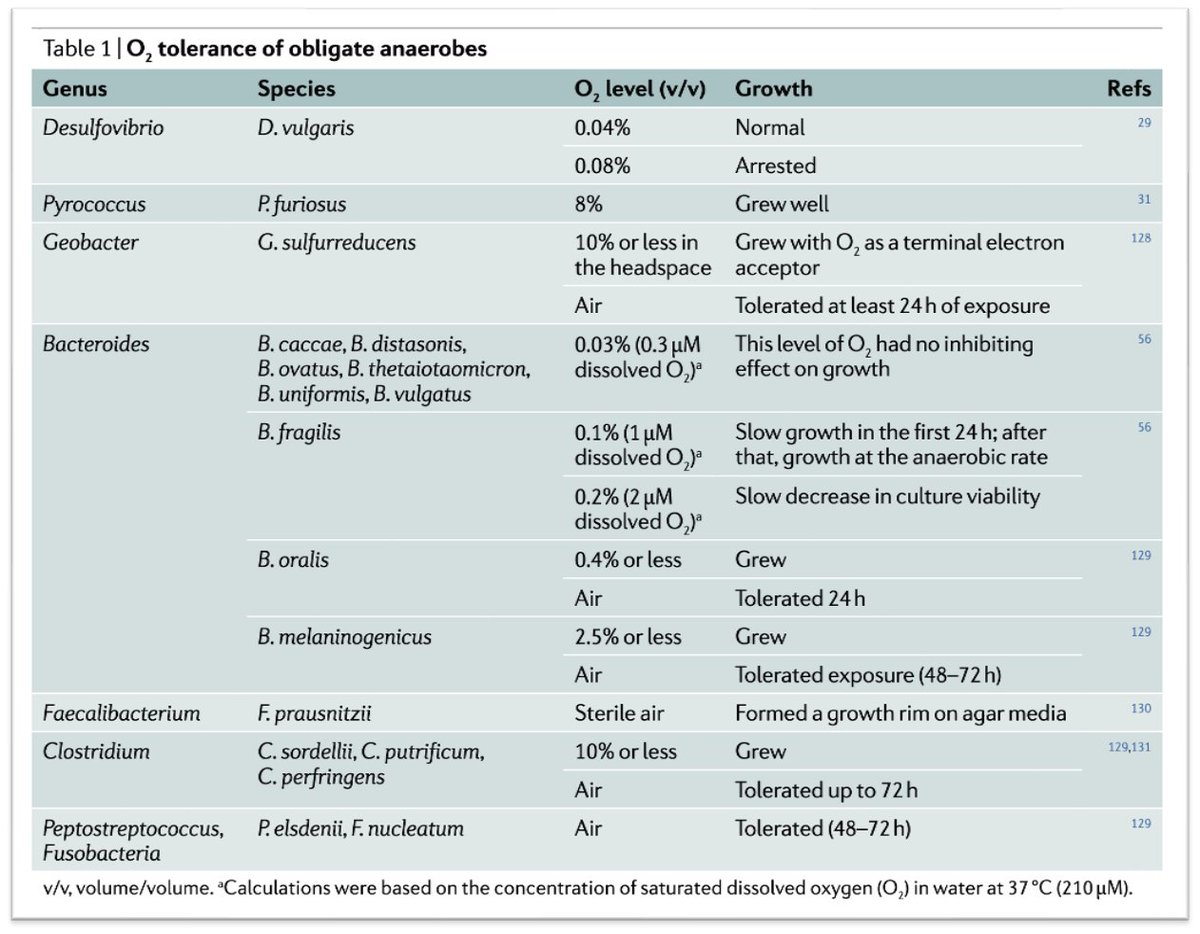
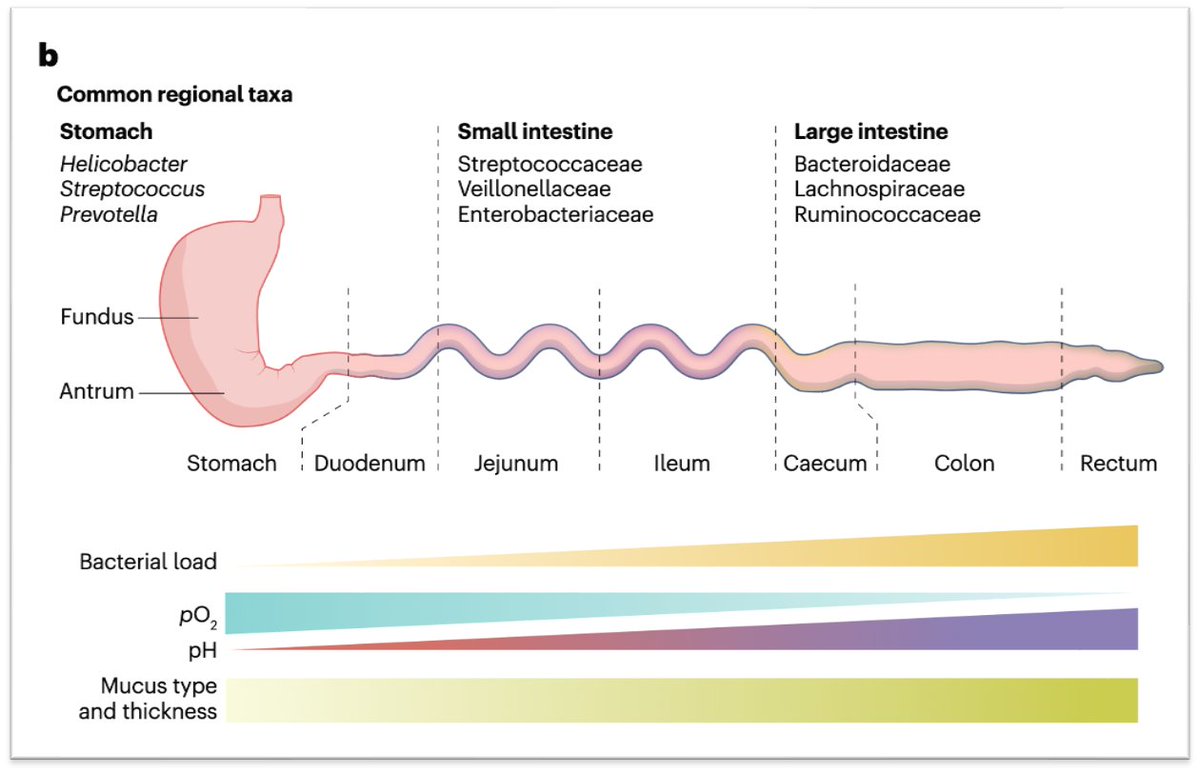
As a reminder, C. difficile is an obligate anaerobe. As with other obligate anaerobes, it prefers environments with low to no oxygen.
This explains why anaerobic bacteria like C. difficile colonize the colon.
pubmed.ncbi.nlm.nih.gov
As a reminder, C. difficile is an obligate anaerobe. As with other obligate anaerobes, it prefers environments with low to no oxygen.
This explains why anaerobic bacteria like C. difficile colonize the colon.
pubmed.ncbi.nlm.nih.gov
4/
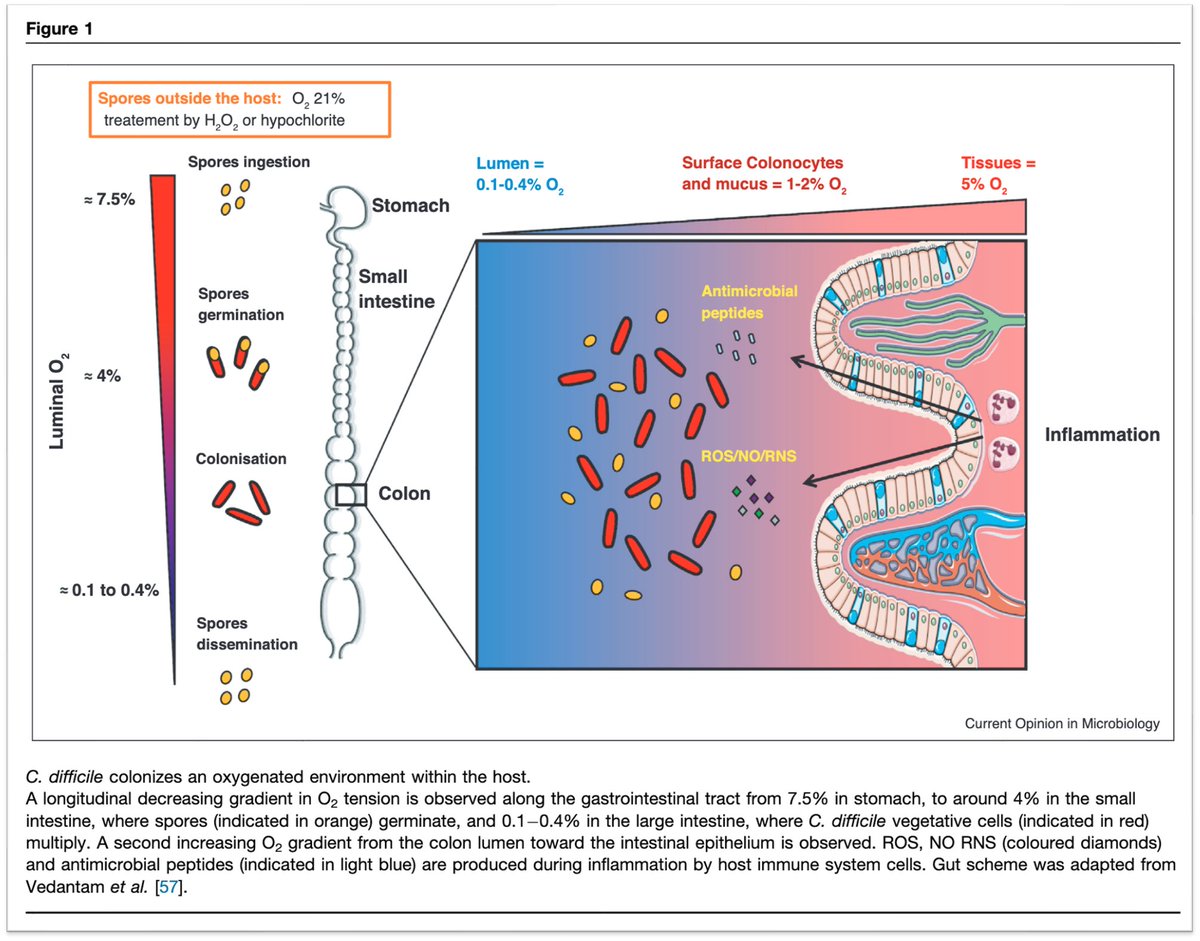
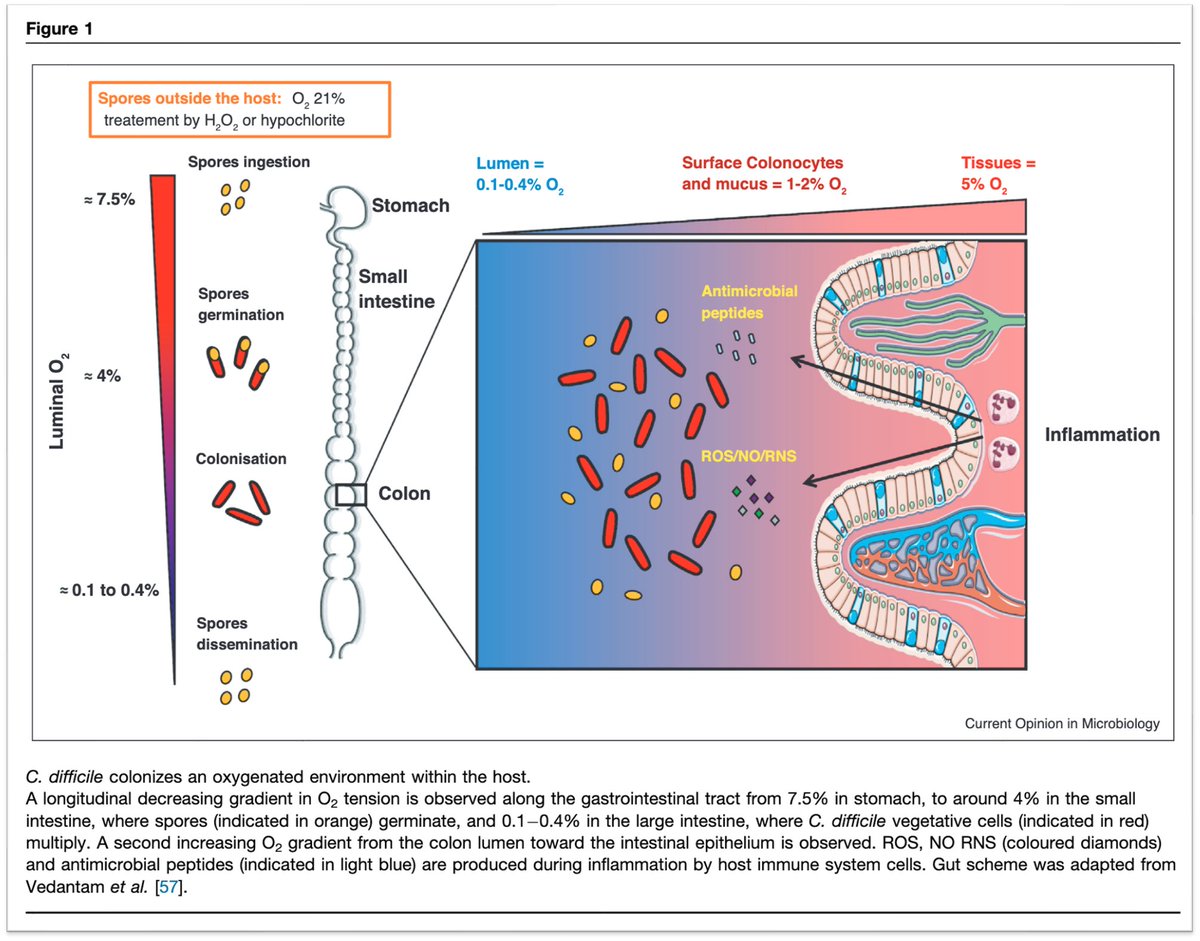
Understanding the geographic predilection of C. difficile requires review of the two oxygen gradients within the gastrointestinal tract.
The first is a luminal gradient from stomach to colon.
➤Stomach 7.5% O₂
➤Small intestine 4%
➤Colon 0.1-0.4%
pubmed.ncbi.nlm.nih.gov
Understanding the geographic predilection of C. difficile requires review of the two oxygen gradients within the gastrointestinal tract.
The first is a luminal gradient from stomach to colon.
➤Stomach 7.5% O₂
➤Small intestine 4%
➤Colon 0.1-0.4%
pubmed.ncbi.nlm.nih.gov
5/
The second oxygen gradient is from intestinal epithelium to lumen.
➤Intestinal epithelium 5% O₂
➤Surface colonocytes and mucus 1-2%
➤Colonic lumen 0.1-0.4%
💡Notice that both gradients end with a colonic lumen that lacks oxygen.
pubmed.ncbi.nlm.nih.gov
The second oxygen gradient is from intestinal epithelium to lumen.
➤Intestinal epithelium 5% O₂
➤Surface colonocytes and mucus 1-2%
➤Colonic lumen 0.1-0.4%
💡Notice that both gradients end with a colonic lumen that lacks oxygen.
pubmed.ncbi.nlm.nih.gov
6/
Obligate anaerobes follow a similar gradient and are found in the greatest number in the colonic lumen.
💡While the small intestine is dominated by facultative anaerobes (e.g., E. coli), 99% of bacterial species in the colon are obligate anaerobes.
pubmed.ncbi.nlm.nih.gov
Obligate anaerobes follow a similar gradient and are found in the greatest number in the colonic lumen.
💡While the small intestine is dominated by facultative anaerobes (e.g., E. coli), 99% of bacterial species in the colon are obligate anaerobes.
pubmed.ncbi.nlm.nih.gov
7/
I suspect the above geography results in two barriers to easy entry of C. difficile into the blood.
(1) It has a "longer" road to travel from lumen to blood than bacteria settled near the epithelium
(2) Along the way, it faces an increasingly inhospitable oxygen tension
I suspect the above geography results in two barriers to easy entry of C. difficile into the blood.
(1) It has a "longer" road to travel from lumen to blood than bacteria settled near the epithelium
(2) Along the way, it faces an increasingly inhospitable oxygen tension
8/
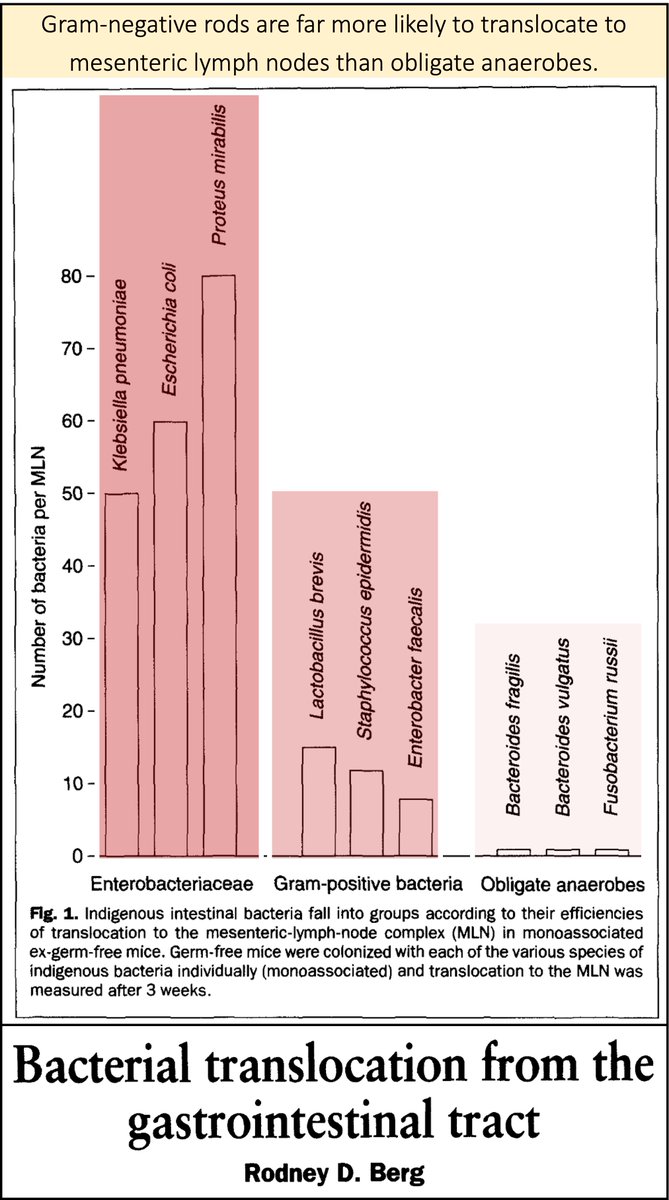
Support for this hypothesis comes from the observation that anaerobic bacteria, like C. difficile, are far less likely to translocate the bowel wall than are facultative anaerobes, like E. coli.
pubmed.ncbi.nlm.nih.gov
Support for this hypothesis comes from the observation that anaerobic bacteria, like C. difficile, are far less likely to translocate the bowel wall than are facultative anaerobes, like E. coli.
pubmed.ncbi.nlm.nih.gov
9/
This helps explain why we don't empirically cover anaerobes when treating spontaneous bacterial peritonitis.
For more on that topic, see this thread.
x.com
This helps explain why we don't empirically cover anaerobes when treating spontaneous bacterial peritonitis.
For more on that topic, see this thread.
x.com
10/
In some ways, my original question might be more appropriately titled, "Why do we EVER see Clostridioides difficile bacteremia?"
If it is so hard to get into the blood AND the blood is oxygenated, shouldn't it be nearly impossible for C. difficile to infect the bloodstream?
In some ways, my original question might be more appropriately titled, "Why do we EVER see Clostridioides difficile bacteremia?"
If it is so hard to get into the blood AND the blood is oxygenated, shouldn't it be nearly impossible for C. difficile to infect the bloodstream?
11/
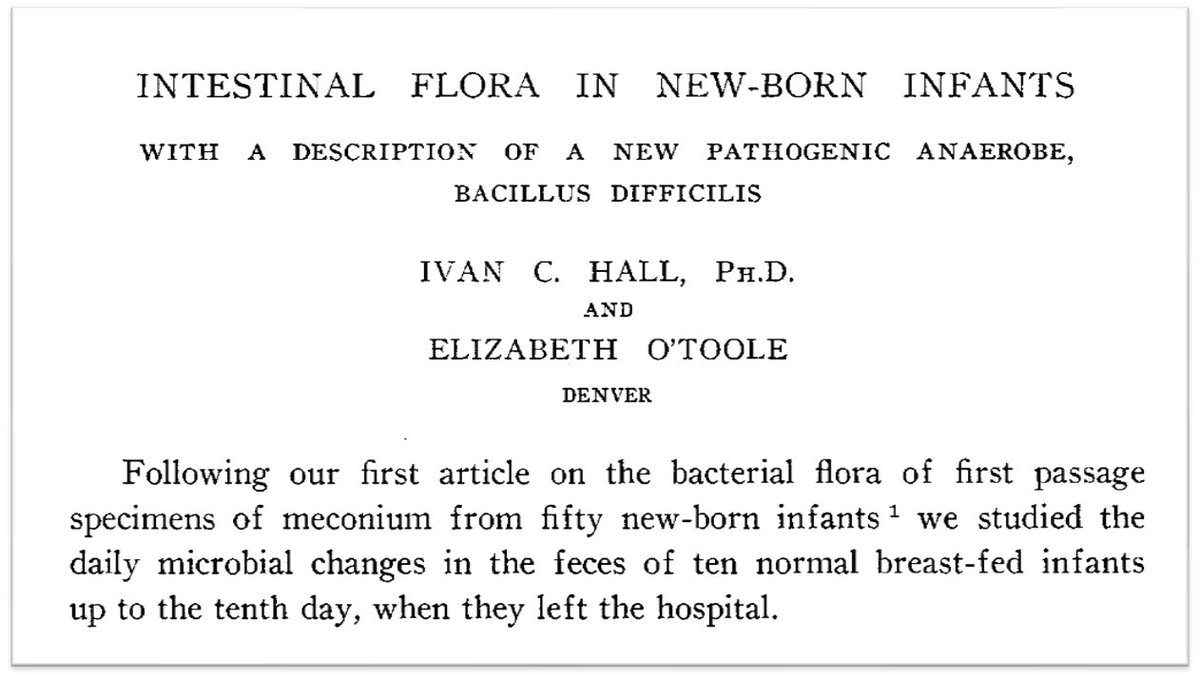
In fact, C. difficile was named specifically as it was hard to isolate.
In their 1935 description, Hall and O'Toole write, "it is therefore named Bacillus difficilis because of the unusual difficulty which was encountered in its isolation and study."
jamanetwork.com
In fact, C. difficile was named specifically as it was hard to isolate.
In their 1935 description, Hall and O'Toole write, "it is therefore named Bacillus difficilis because of the unusual difficulty which was encountered in its isolation and study."
jamanetwork.com
12/
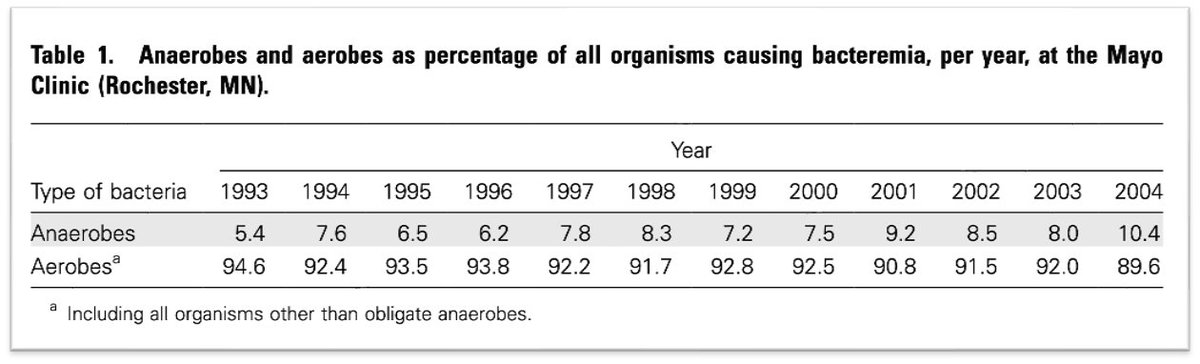
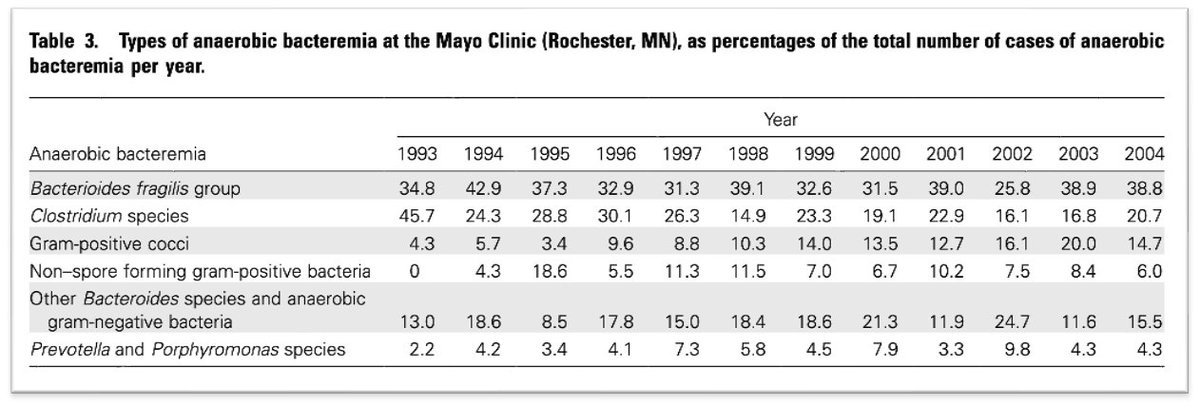
But other anaerobes DO infect the blood.
💡Cohort studies suggest anaerobic bacteria cause 5-10% of bloodstream infections.
pubmed.ncbi.nlm.nih.gov
But other anaerobes DO infect the blood.
💡Cohort studies suggest anaerobic bacteria cause 5-10% of bloodstream infections.
pubmed.ncbi.nlm.nih.gov
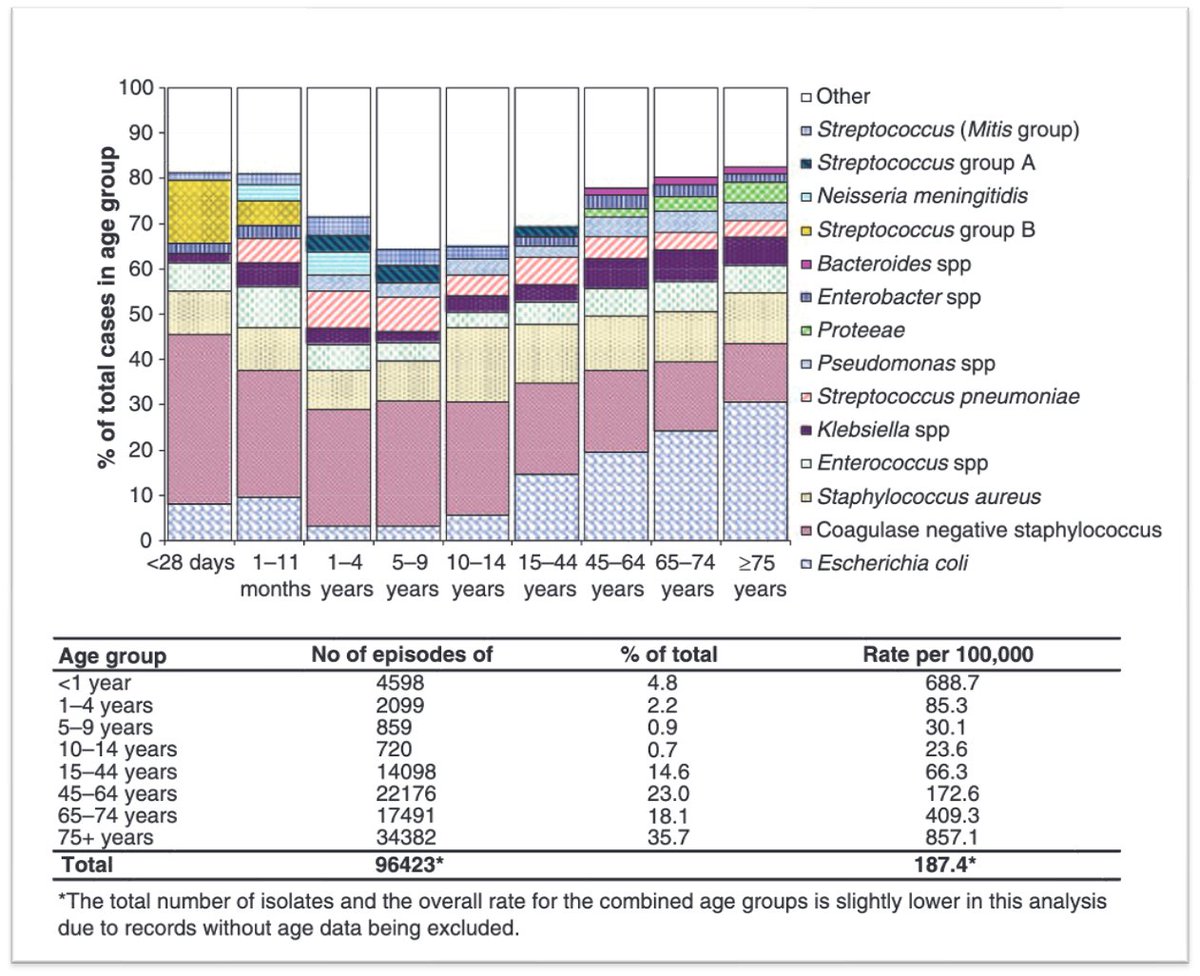
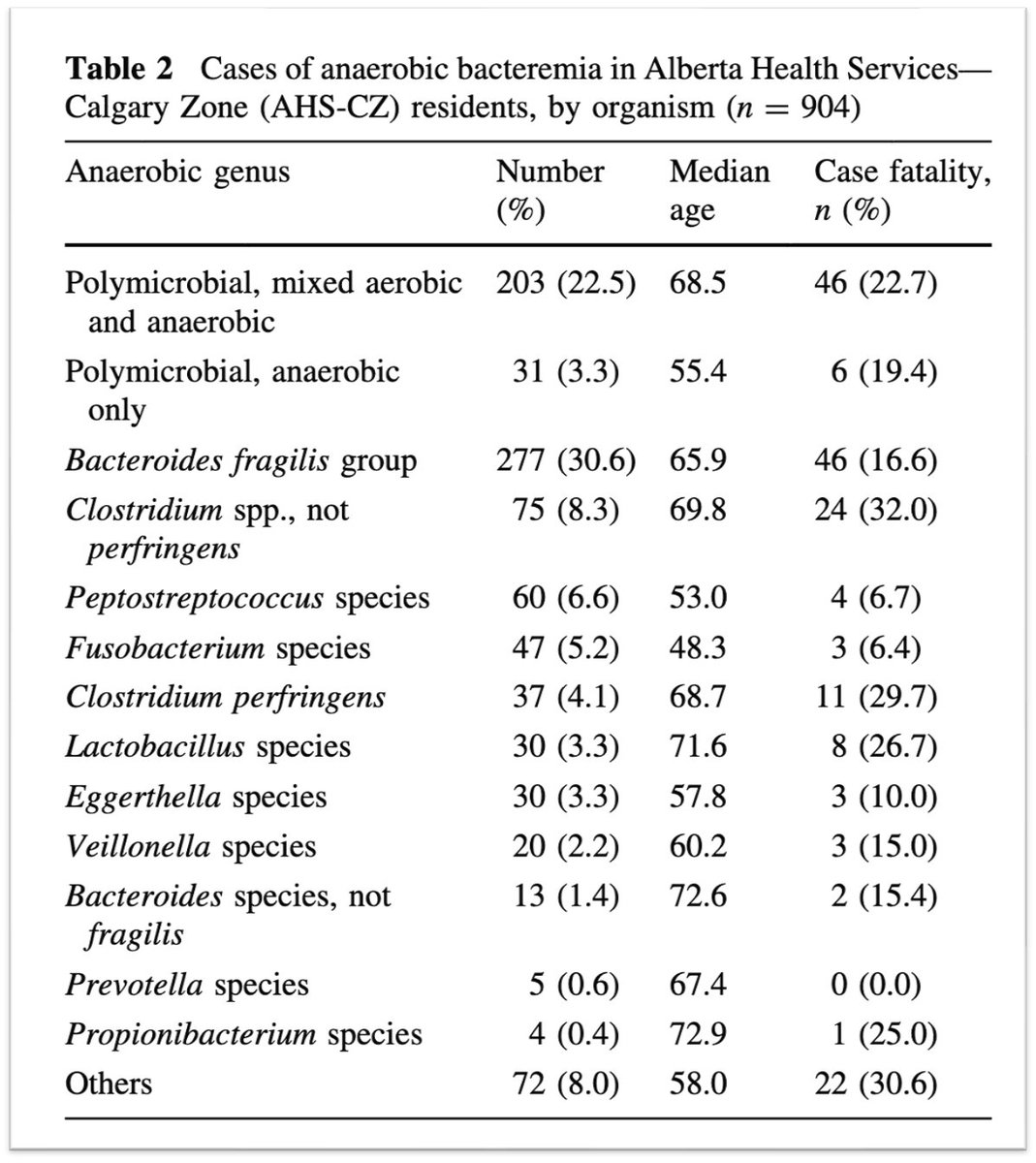
13/
E. coli is the most common cause of bacteremia overall.
Among obligate anaerobes, Bacteroides species top the list.
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
E. coli is the most common cause of bacteremia overall.
Among obligate anaerobes, Bacteroides species top the list.
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov/20491834/
Trends among pathogens reported as causing bacteraemia in England, 2004-2008 - PubMed
The Health Protection Agency in England operates a voluntary surveillance system that collects data...

pubmed.ncbi.nlm.nih.gov/17342637/
Reemergence of anaerobic bacteremia - PubMed
Anaerobic bacteremia has reemerged as a significant clinical problem. Although there are probably mu...
14/
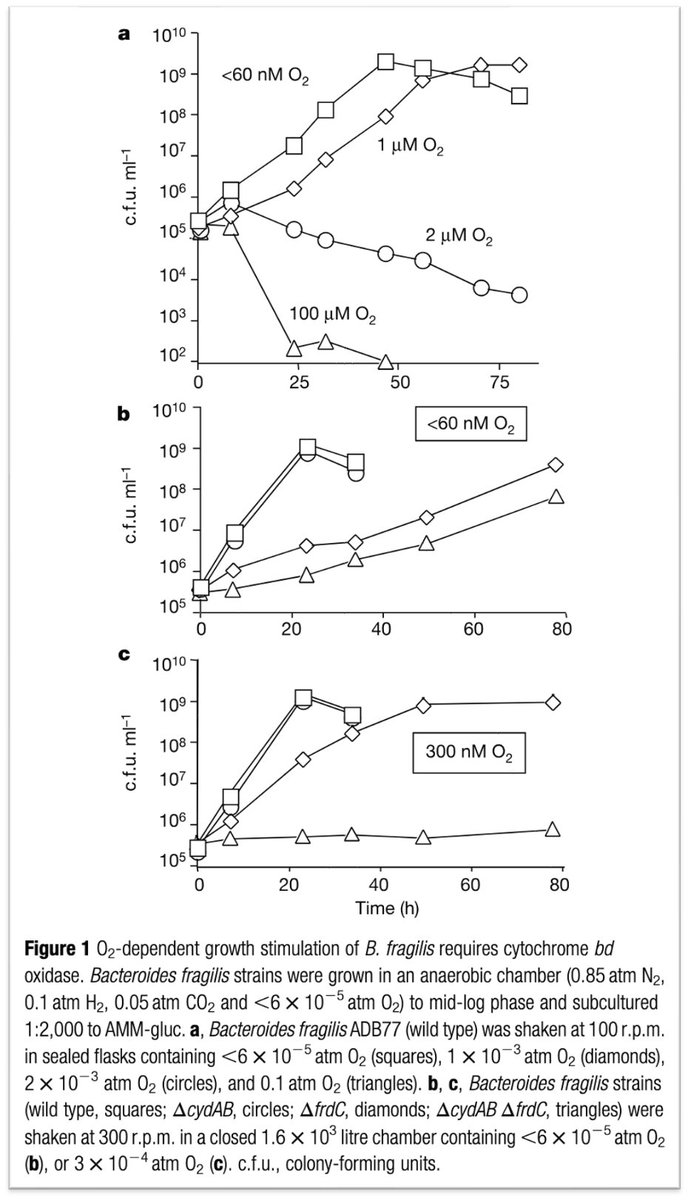
Bacteroides fragilis is interesting. Although it is an obligate anaerobe, it can use oxygen as a terminal electron acceptor at nanomolar concentrations.
This may help explain why it is the most common obligate anaerobe to be isolated in the blood.
pubmed.ncbi.nlm.nih.gov
Bacteroides fragilis is interesting. Although it is an obligate anaerobe, it can use oxygen as a terminal electron acceptor at nanomolar concentrations.
This may help explain why it is the most common obligate anaerobe to be isolated in the blood.
pubmed.ncbi.nlm.nih.gov
15/
Even C. difficile can grow at low oxygen tensions.
Studies have shown that the bacterium can grow in 1-3% oxygen and tolerate brief air exposure.
ncbi.nlm.nih.gov
Even C. difficile can grow at low oxygen tensions.
Studies have shown that the bacterium can grow in 1-3% oxygen and tolerate brief air exposure.
ncbi.nlm.nih.gov
16/
Despite its ability to grow in the presence of oxygen, C. difficile is far less commonly isolated from the blood than other Clostridial species, like Clostridium perfringens.
pubmed.ncbi.nlm.nih.gov
Despite its ability to grow in the presence of oxygen, C. difficile is far less commonly isolated from the blood than other Clostridial species, like Clostridium perfringens.
pubmed.ncbi.nlm.nih.gov
17/
Why C. difficile is less able to proliferate in the blood compared with C. perfringens is not entirely unclear.
I wasn't able to find any definitive explanations.
What have I missed?
Why C. difficile is less able to proliferate in the blood compared with C. perfringens is not entirely unclear.
I wasn't able to find any definitive explanations.
What have I missed?
18/18
𖠘 Clostridioides difficile is a rare cause of bloodstream infections
𖠘 This is likely explained, in part, by the fact that it is an obligate anaerobe
𖠘 Other obligate anaerobes can proliferate more easily; why C. difficile has such a "hard time" in the blood is unclear
𖠘 Clostridioides difficile is a rare cause of bloodstream infections
𖠘 This is likely explained, in part, by the fact that it is an obligate anaerobe
𖠘 Other obligate anaerobes can proliferate more easily; why C. difficile has such a "hard time" in the blood is unclear
جاري تحميل الاقتراحات...