(1/6): 5 myths of IV fluids 🦄
A 🧵that makes my soul cringe.
Please help spread the word 🙏#stopinhospitaldrowning
A 🧵that makes my soul cringe.
Please help spread the word 🙏#stopinhospitaldrowning
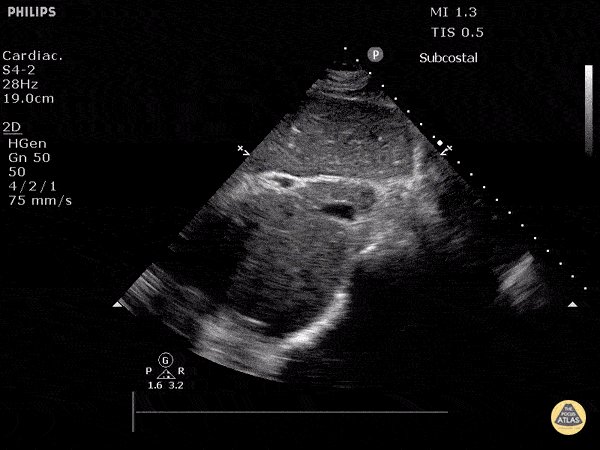
(2/6) Myth 1: You should resuscitate and "fill up" the IVC - "there is still room based on the IVC to give fluids..."
Response: We are not car mechanics filling up oil 🛢️
Response 2: IVC can be flat in hypovolemia OR distributive shock OR normal healthy state and does NOT predict fluid responsiveness 🚫
IVC needs to be decoupled entirely from fluid responsiveness. Yes it can tell us a little about tolerance, but NOT responsiveness. ❗️
Response: We are not car mechanics filling up oil 🛢️
Response 2: IVC can be flat in hypovolemia OR distributive shock OR normal healthy state and does NOT predict fluid responsiveness 🚫
IVC needs to be decoupled entirely from fluid responsiveness. Yes it can tell us a little about tolerance, but NOT responsiveness. ❗️
(4/6) Myth 3: My patient’s kidneys are "borderline" - if I don't give them enough fluid they will fail.
Response: IV fluids are not intrinsically beneficial to kidneys. They only help kidneys if the patient is fluid responsive and fluid tolerant. IV fluids can worsen venous congestion and kidney failure
Response: IV fluids are not intrinsically beneficial to kidneys. They only help kidneys if the patient is fluid responsive and fluid tolerant. IV fluids can worsen venous congestion and kidney failure
Loading suggestions...



![(6/6) Myth 5: I just use [x test] to tell if my patient is dry
Insert the following as [x test]: Sw...](https://pbs.twimg.com/media/GFH6HUwWwAELWd4.jpg)