1/
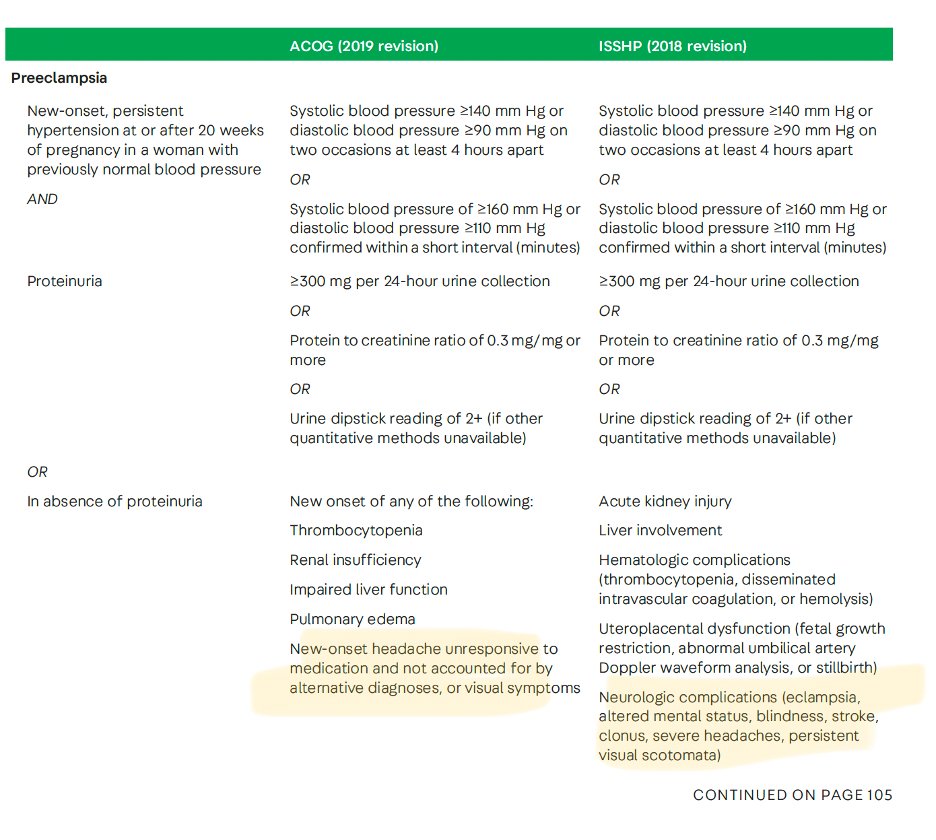
A 21 yo G1P0 reports a severe headache 3 days after delivery.
BP 182/100😱
While waiting to be admitted, she vomits & has a generalized tonic clonic seizure.
She is sedated and intubated for eclampsia.
The next morning, she has blown pupils.
A #continuumcase. @LyellJ
A 21 yo G1P0 reports a severe headache 3 days after delivery.
BP 182/100😱
While waiting to be admitted, she vomits & has a generalized tonic clonic seizure.
She is sedated and intubated for eclampsia.
The next morning, she has blown pupils.
A #continuumcase. @LyellJ
2/
(What happened to cases from the sleep issue, you ask!?
We’ll get back there, but I’m reviewing the 2022 issue on the neurology of pregnancy for the EB meeting… )
Didn't you want some tips on neuro-emergencies in pregnancy?
(What happened to cases from the sleep issue, you ask!?
We’ll get back there, but I’m reviewing the 2022 issue on the neurology of pregnancy for the EB meeting… )
Didn't you want some tips on neuro-emergencies in pregnancy?
3/
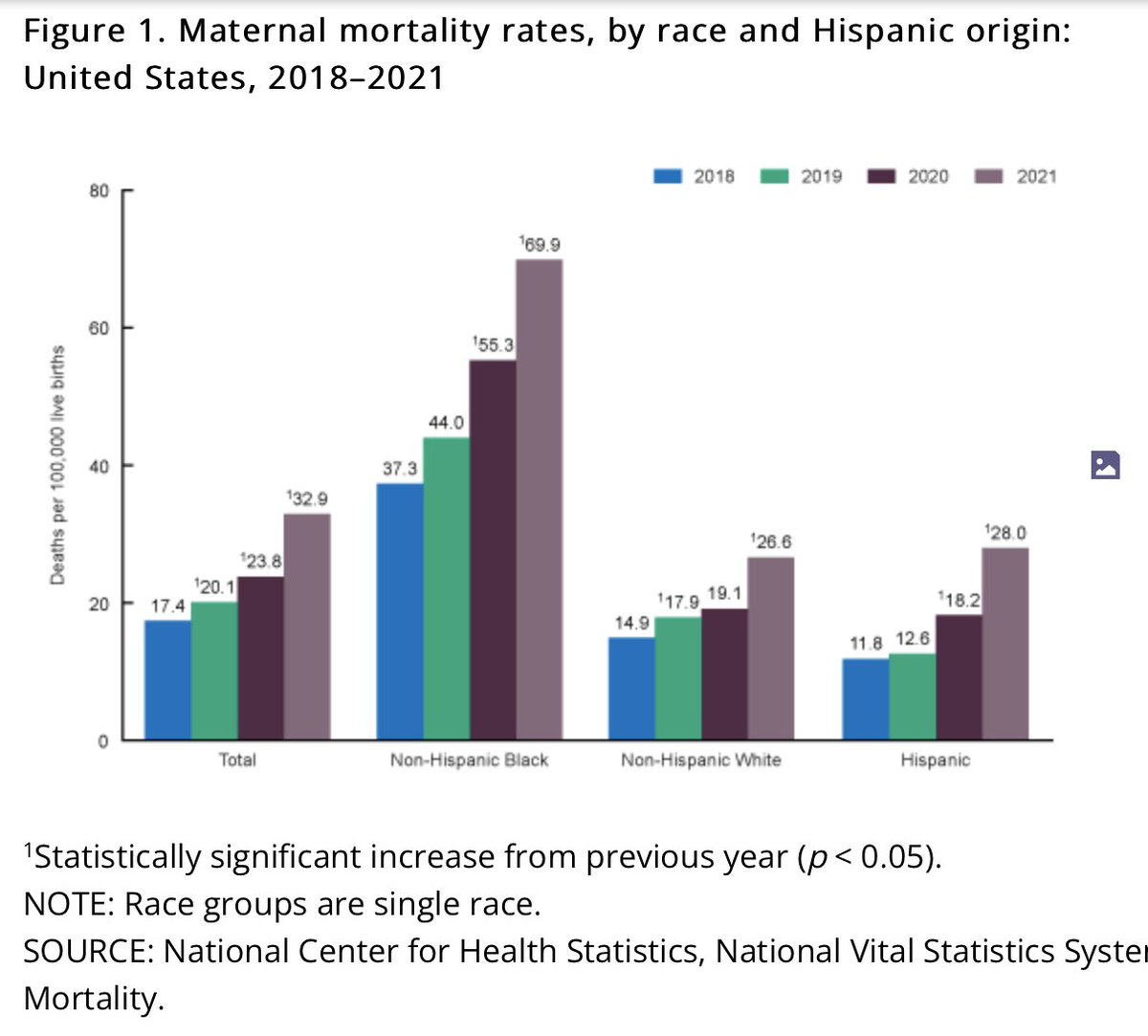
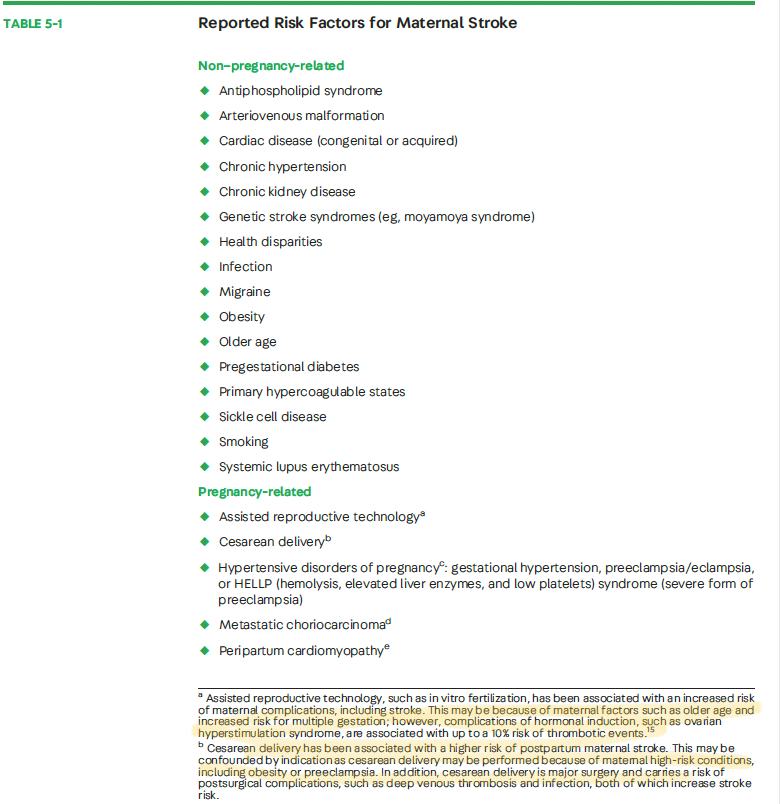
Pregnancy is a very scary time (having just been there myself I can confirm there seems to always be something to worry about!).
🤰Pregnancy TRIPLES the incident of stroke (compared to non-preg women childbearing age)
🤰Maternal stroke complicates 30 of 100,000 deliveries!!
Pregnancy is a very scary time (having just been there myself I can confirm there seems to always be something to worry about!).
🤰Pregnancy TRIPLES the incident of stroke (compared to non-preg women childbearing age)
🤰Maternal stroke complicates 30 of 100,000 deliveries!!
4/
If you have a high-risk, comorbidity like hypertensive disorder of pregnany, the stroke incident may be as high as 1 in 500 deliveries.
PLUS, half of maternal strokes are hemorrhagic stroke: 👉carries a higher risk of morbidity
👉up to 50% are fatal.
If you have a high-risk, comorbidity like hypertensive disorder of pregnany, the stroke incident may be as high as 1 in 500 deliveries.
PLUS, half of maternal strokes are hemorrhagic stroke: 👉carries a higher risk of morbidity
👉up to 50% are fatal.
7/
Although 'pregnancy' is the risk factor, most stroke occur AFTER delivery.
🩸First 2 weeks=highest risk period
🩸Maternal thromboembolic events & ICH remain definitively elevated for up to 12 weeks
& May be elevated for a full year after delivery! pubmed.ncbi.nlm.nih.gov
Although 'pregnancy' is the risk factor, most stroke occur AFTER delivery.
🩸First 2 weeks=highest risk period
🩸Maternal thromboembolic events & ICH remain definitively elevated for up to 12 weeks
& May be elevated for a full year after delivery! pubmed.ncbi.nlm.nih.gov
8/
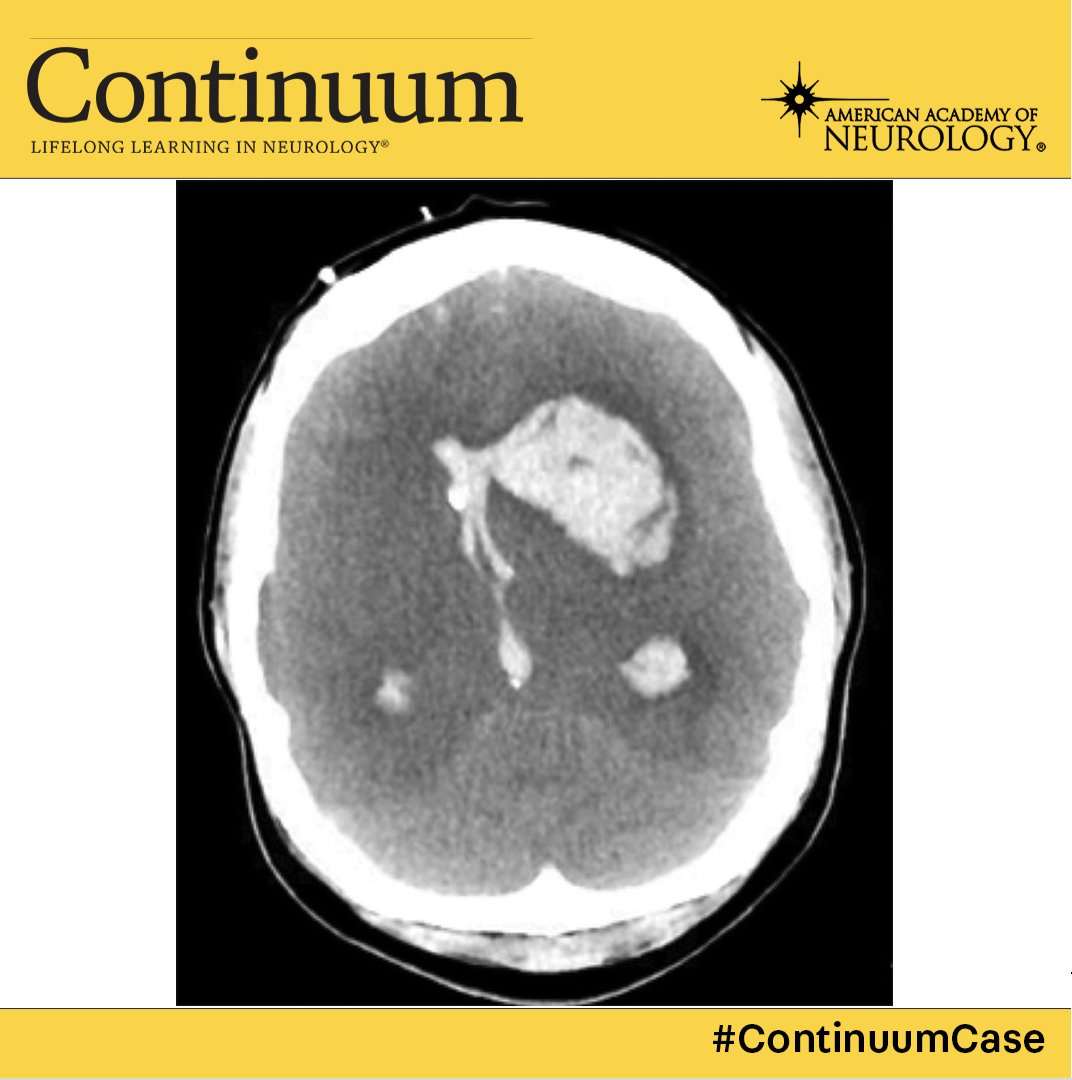
Back to this case.
The patient had seizure like movements and was thought to have eclampsia.
But louder now, for the people in the back.
NOT ALL THAT SHAKES IS SEIZURE!
The availability of “loss of consciousness+hyperkinetic movement ”=“eclampsia” makes for an easy⚓️ point
Back to this case.
The patient had seizure like movements and was thought to have eclampsia.
But louder now, for the people in the back.
NOT ALL THAT SHAKES IS SEIZURE!
The availability of “loss of consciousness+hyperkinetic movement ”=“eclampsia” makes for an easy⚓️ point
9/
But -- if the eclamptic patient doesn’t rapidly return to baseline, they need a stat CT *AND* CTA!
⏰ CT for ?hemorrhage
⏰ CTA because nothing is worse than realizing too late that the altered patient has a basilar thrombus.
But -- if the eclamptic patient doesn’t rapidly return to baseline, they need a stat CT *AND* CTA!
⏰ CT for ?hemorrhage
⏰ CTA because nothing is worse than realizing too late that the altered patient has a basilar thrombus.
10/
Is this safe in pregnancy?
Yes.
👉Current CTs deliver up to 0.1mGy (far < 50 mGy threshold)
👉Contrast has a theoretic risk of neonatal hypothyroidism, but that risk is outweighed by the benefit of diagnosis acute stroke.
MRIs are also ok.
gadolinium = avoid if possible.
Is this safe in pregnancy?
Yes.
👉Current CTs deliver up to 0.1mGy (far < 50 mGy threshold)
👉Contrast has a theoretic risk of neonatal hypothyroidism, but that risk is outweighed by the benefit of diagnosis acute stroke.
MRIs are also ok.
gadolinium = avoid if possible.
13/
what about hyperosmolar therapy?
Not a lot of data.
But, if the patient is still pregnant:
mannitol 0.25-0.5g/kg is considered safe
HTS can be considered but safety is less well established
what about hyperosmolar therapy?
Not a lot of data.
But, if the patient is still pregnant:
mannitol 0.25-0.5g/kg is considered safe
HTS can be considered but safety is less well established
15/
There are so many awesome and informative @ContinuumAAN articles, but this one by @ElizaMillerMD is really a *standout* and these are complex, young patients. truly, a must read.
journals.lww.com
There are so many awesome and informative @ContinuumAAN articles, but this one by @ElizaMillerMD is really a *standout* and these are complex, young patients. truly, a must read.
journals.lww.com
Loading suggestions...