🤩Good morning #NephTwitter!
Let’s discuss the management of heart failure in patients with kidney disease!
👋I am @HDiniz_ and I will guide you through the latest evidence from the ESC guidelines and beyond.
🧵6 min read👇👇👇
Let’s discuss the management of heart failure in patients with kidney disease!
👋I am @HDiniz_ and I will guide you through the latest evidence from the ESC guidelines and beyond.
🧵6 min read👇👇👇
Did you know that HF affects > 10% of patients over 65+? 💔
HF & CKD are like BFFs, sharing risk factors & heart quirks 😎
This overlap leads to the very common CKD-associated cardiomyopathy!
HF & CKD are like BFFs, sharing risk factors & heart quirks 😎
This overlap leads to the very common CKD-associated cardiomyopathy!
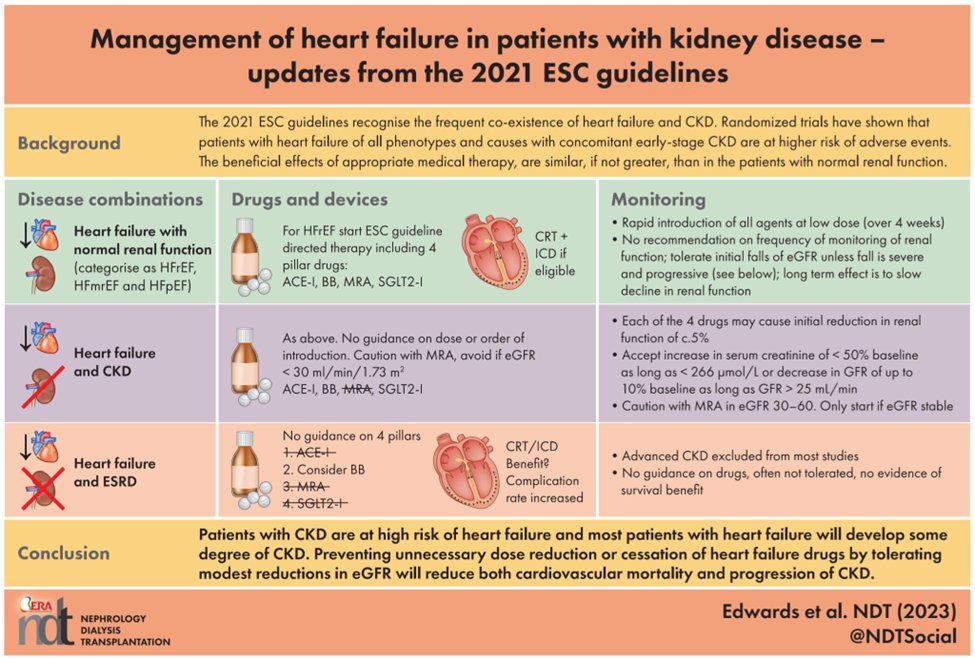
RCTs are clear. HF-GDT works wonders in mild-moderate CKD! 🥳
The ESC guidelines stress the long term benefits on prognosis and kidney function in HF.📉
But advanced CKD pts are MIA in these studies, leaving a treatment gap! 😟
The ESC guidelines stress the long term benefits on prognosis and kidney function in HF.📉
But advanced CKD pts are MIA in these studies, leaving a treatment gap! 😟
HF Diagnosis? 💔
Looks for dyspnea, edema & fatigue - familiar right? Cuz’ they are also associated with CKD 😕
Dx needs backup: EKG, BNP, echo & CXR (May I add Lung Ultrasound? 😆 #POCUS)
Looks for dyspnea, edema & fatigue - familiar right? Cuz’ they are also associated with CKD 😕
Dx needs backup: EKG, BNP, echo & CXR (May I add Lung Ultrasound? 😆 #POCUS)
But Echo’s the MVP - measures LVEF and stratifies HF types! Ready for some EF math? 🧮
- HFrEF (<40%)
- HFmrEF (41-49%)
- HFpEF (>50%)
- HFrEF (<40%)
- HFmrEF (41-49%)
- HFpEF (>50%)
Natriuretic peptides are great!
Check this out: NT-proBNP < 125 pg/ml = HF is a long shot.
And the magnitude of elevation is also of prognostic value 🔮
No specific guidance on the use of BNP in patients with CKD 😟
But with eGFR > 30, there’s no need to worry.
Check this out: NT-proBNP < 125 pg/ml = HF is a long shot.
And the magnitude of elevation is also of prognostic value 🔮
No specific guidance on the use of BNP in patients with CKD 😟
But with eGFR > 30, there’s no need to worry.
Natriuretic peptides standard cut-off holds its group till CKD G4. But in dialysis patients, BNP waves warning flags for mortality (and maybe congestion?), not HF diagnosis!
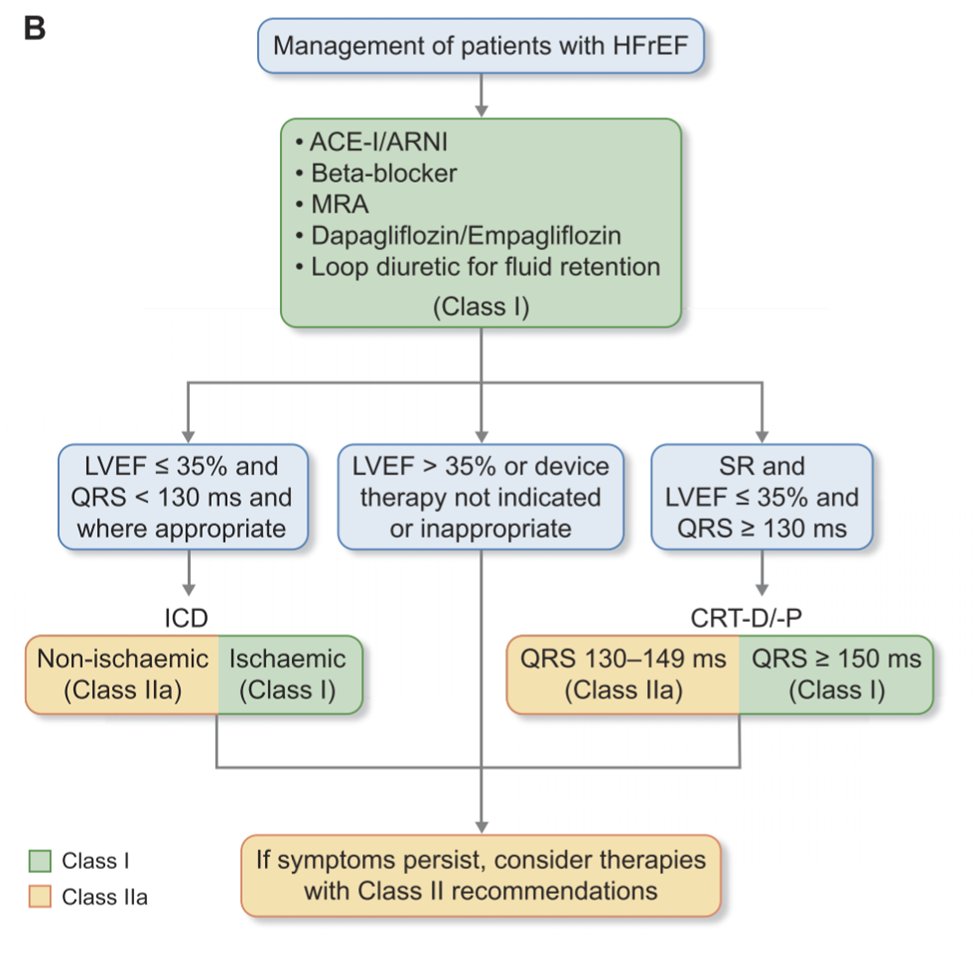
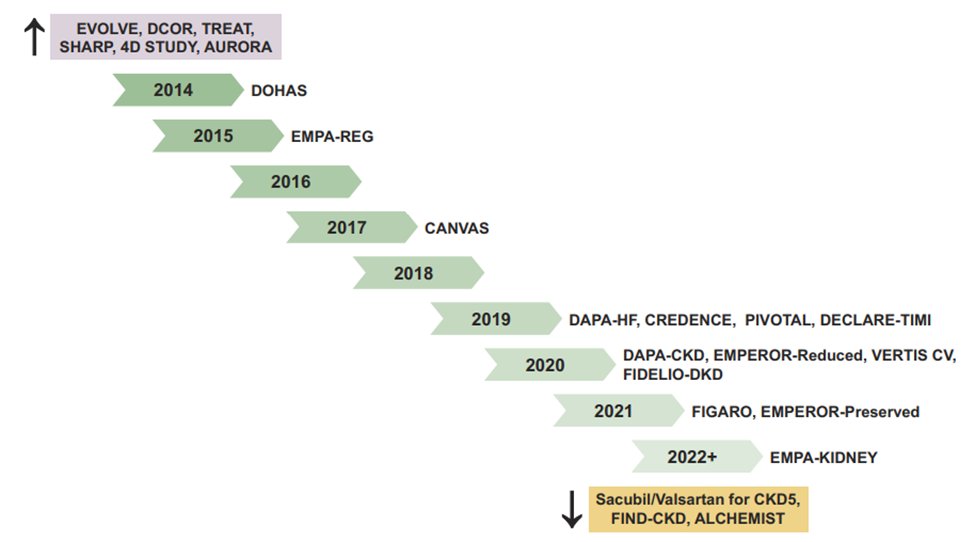
HF treatment evolution ✊🏽
HFrEF? We got it covered, thanks to 40 years of trial magic 🪄 HFmrEF & HFpEF are trickier due to variety & comorbidities.
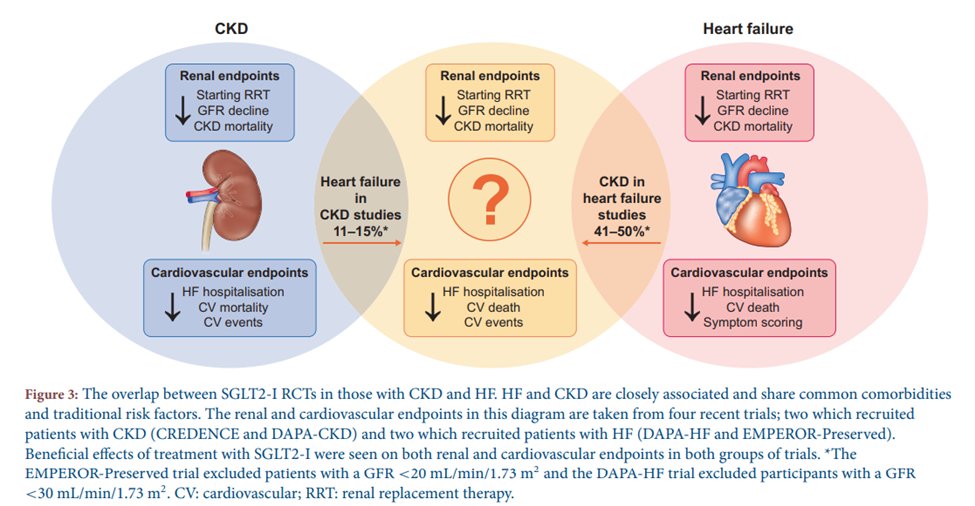
Say hello to SGLT2i!
They aimed at sugar but hit the heart and kidneys!
HFrEF? We got it covered, thanks to 40 years of trial magic 🪄 HFmrEF & HFpEF are trickier due to variety & comorbidities.
Say hello to SGLT2i!
They aimed at sugar but hit the heart and kidneys!
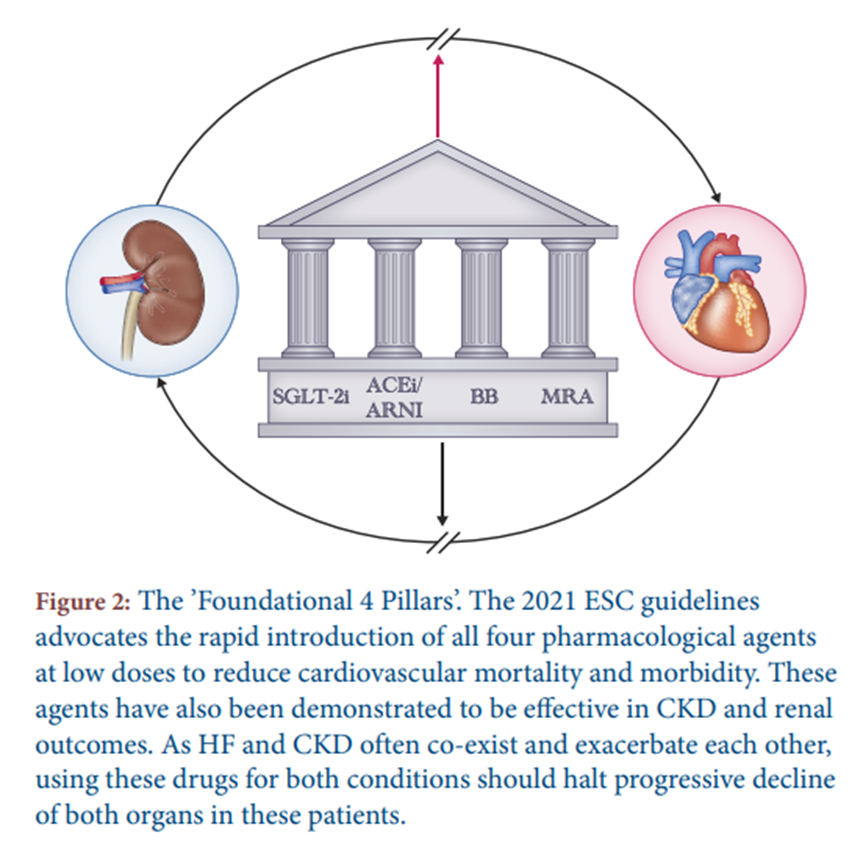
Why? Slow titration is > 6-month journey. Low doses of 4 agents >> one’s high dose. This data is consistent across the board: even with small doses come big benefits reflecting different mechanisms of action! 🏺
Each pillar’s magic stands on its own. Plus, bonus point? Early separation of Kaplan-Meier curves on mortality and morbidity, as early as 30 days! 📈
Also, this strategy is safer with lower rates of kidney dysfunction and HiperK+ 🍌
Also, this strategy is safer with lower rates of kidney dysfunction and HiperK+ 🍌
Kidney worries? Don’t stress. GFR dips don’t mean you have to give up. Here’s the deal:
Creatinine ⬆️ <50% or eGFR ⬇️ < 10% from baseline is OK. In the long run, the pillar meds will keep the kidneys happy, slowing CKD progression and proteinuria.
Creatinine ⬆️ <50% or eGFR ⬇️ < 10% from baseline is OK. In the long run, the pillar meds will keep the kidneys happy, slowing CKD progression and proteinuria.
HFpEF is a complex conundrum but accounts for, at least, 50% of cases of patients with CKD 💝
Besides SGLT2i proven-benefits, there are some interesting signals from sub-analysis from trials of spironolactone & ARNI that could support the use of these drugs in clinical practice.
Besides SGLT2i proven-benefits, there are some interesting signals from sub-analysis from trials of spironolactone & ARNI that could support the use of these drugs in clinical practice.
Device therapy like pacemakers is estimated at only 5-10% in CKD cohorts. There is no proven survival benefit of ICDs in eGFR < 35 ml/min (competing risk for non-arrhythmic death?). In dialysis hearts, ICDs are disappointing too and associated with a high rate of AE!
Functional iron deficiency (ID) is a very common problem in both HF and CKD. ID spells trouble even without anemia. IV iron ⬇️ admissions for HF, ⬆️ symptom burden and QoL!
Screen for ID periodically! 🧪
Screen for ID periodically! 🧪
Recent trials like IRONMAN & AFFIRM-AHF echo IV iron’s value. In advanced CKD new evidence alleviates previous concerns like Vascular calcification or Infection risk. PIVOTAL even showed a in ⬇️ HF admissions and death in dialysis patients! 🏥
#NephTwitter should take the chance to familiarize themselves with the ESC guidelines and the evolving evidence-based landscape in cardiorenal medicine lead by
SGLT2i, non-steroidal MRA and IV iron.
The challenge is to translate these findings into timely guidance for clinicians!
SGLT2i, non-steroidal MRA and IV iron.
The challenge is to translate these findings into timely guidance for clinicians!
Did you enjoy this kind of educational content?
Check out the full paper, discuss and follow @NDTSocial for more!
academic.oup.com
Check out the full paper, discuss and follow @NDTSocial for more!
academic.oup.com
Loading suggestions...