Guess what got me into vascular neurology? A tweetorial below hoping to spark your interest as well... this is my understanding/perception based on available data @meded @medtwitter #stroke #Neurology
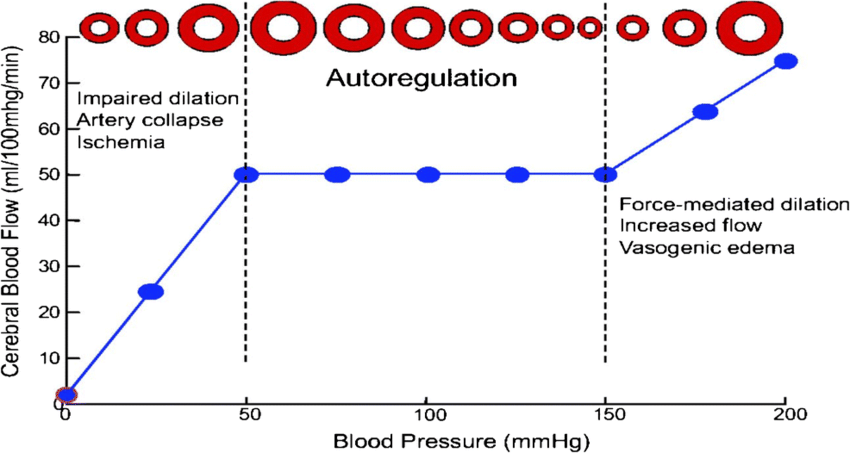
Stage 1 is autoregulation/collateral compensation. In this stage the arterioles may dilate to increase CBV and CBF remains normal. Arterioles are NOT maximally dilated here and there is still cerebovascular reserve. link.springer.com
Also, the collaterals can kick in & compensate without the need for autoregulation. For example, in patients with unilateral carotid occlusion, the collateral circulation through the ACOM or PCOM can compensate without the need to vasodilate. These are first lines of defense.
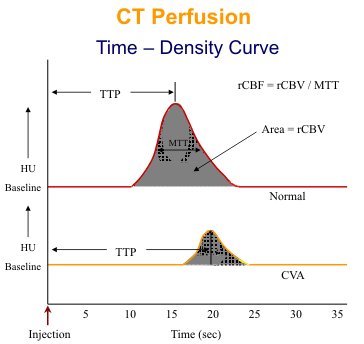
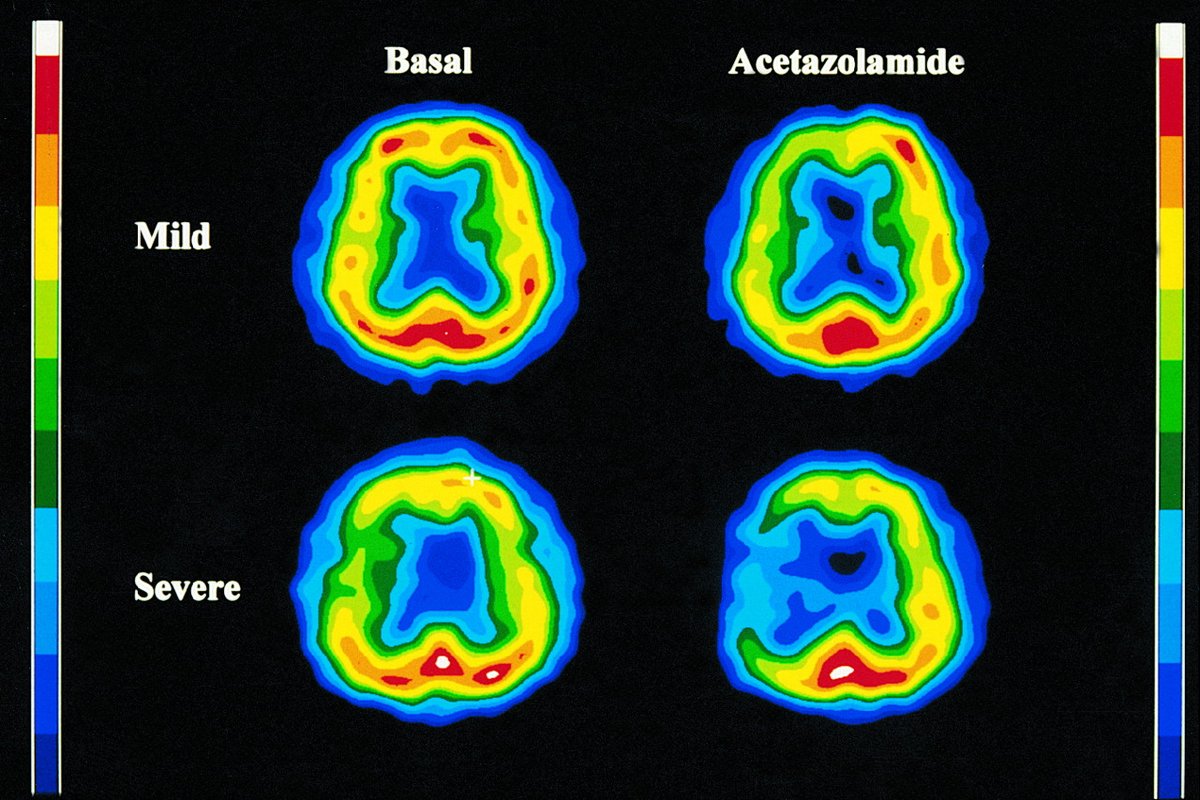
How to test reserve? Diamox SPECT or TCD w CO2. Diamox dilates arterioles inc CBV & CBF. If no increase seen, then the arterioles are maximally dilated & this is beyond stage I. CBF can go down in severe hemodynamic failure (reverse robin-hood phenomenon)! jnm.snmjournals.org
You can also do a TCD w CO2 or breath holding. inc CO2 -> arteriolar dilation -> increase velocity across the artery due to reduction in downstream resistance. Yes increase by 2% or more (not decrease!). If no 2% increase or a decrease, this indicates no reserve/maximal dilation.
Stage II = oligemia (CBF 20-50). Oligemic brain operates normally by extracting more O2 to keep CMRO2 nl. CMRO2 is affected by CBF, OEF, & Hb. CBV goes up here and so does OEF. Any challenge (i.e. lowering BP) could bring on symptoms. Check this review out ahajournals.org
Stage III = penumbra or electrical failure. A stage of hibernation due to low ATP. CBF = 10-20. The area is symptomatic but could be revived with timely reperfusion. CMRO2 is reduced. Brain tissue cannot hibernate forever & will eventually die off if no reperfusion. Time = Brain!
Stage 4 = infarct (CBF<10). Neurons operate based on Na & K (depolarization/repolarization). The Na/K ATPase needs ATP to keep Na out; Na in ->water in ->swelling/ cell death. ATP is formed by Glucose+O2 thru glycolysis/krebs cycle/electron transport. CBF<10 = no gluc/O2 = no ATP
Acutely, the 4 stages can exist in the same person. With time, part of the penumbra dies off and the other part becomes stage I or II tissue. And chronically there are usually up to three stages (infarct, oligemia, and autoregulation).
Finally, my theory is that there is always a core. Tools to measure it are imperfect. 7T or more MRI/serum biomarkers may measure microscopic brain injury but this needs more study. These will help diagnose ischemia in patients with transient sxs & then we can retire the term TIA
If you found this helpful, please RT. @caseyalbin @MicieliA_MD @a_charidimou @StrokeAHA_ASA @rkchoi #MedEd #NeuroTwitter #stroke
Loading suggestions...