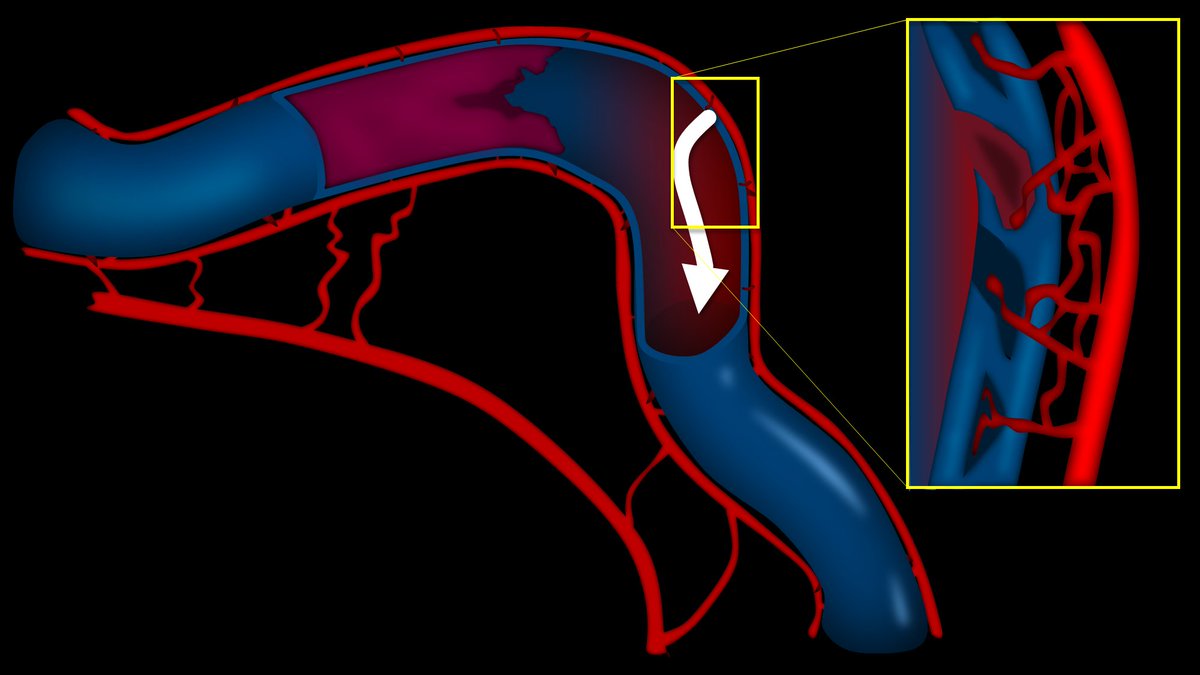
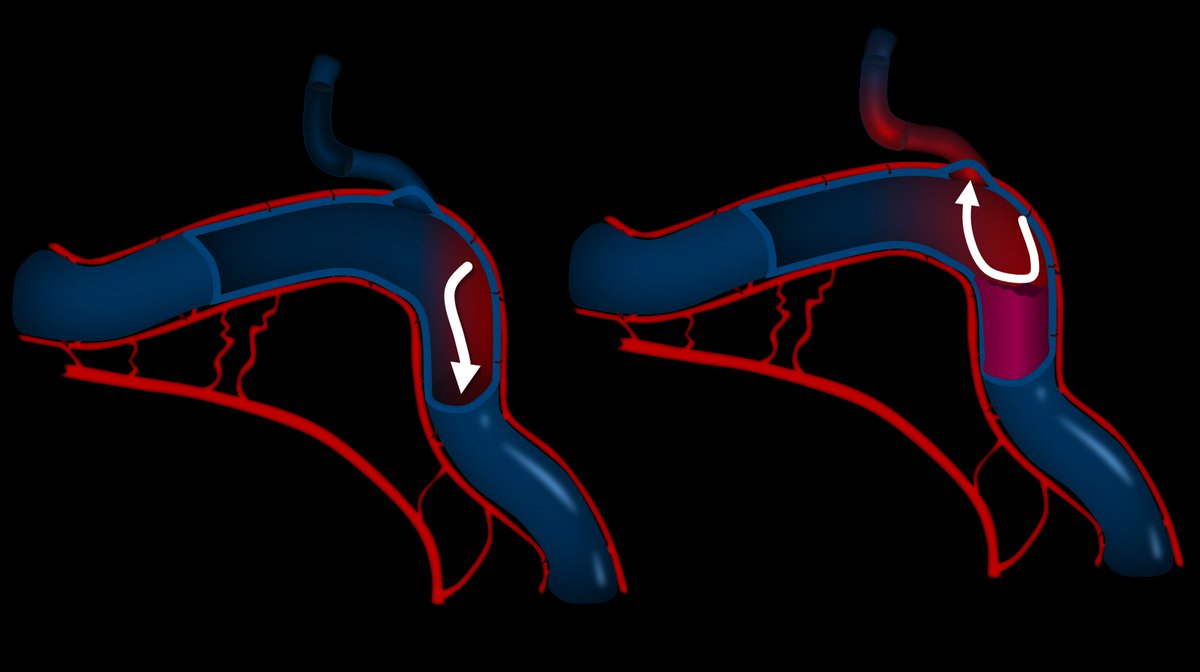
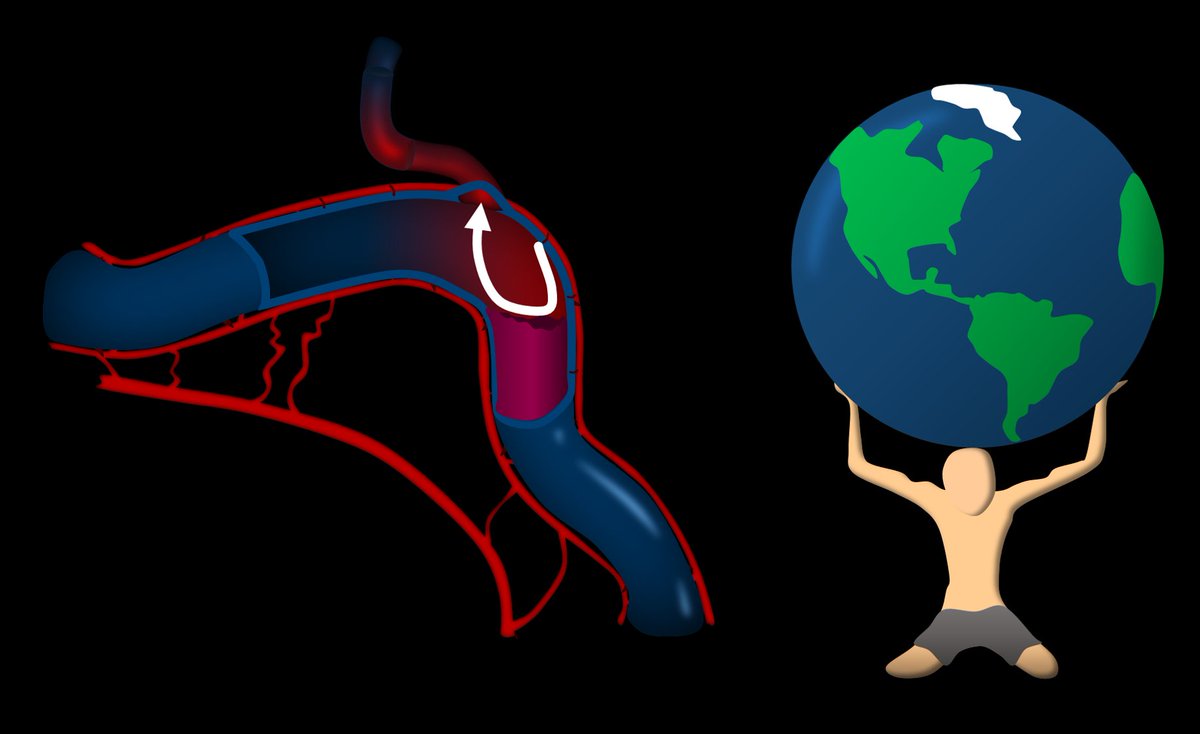
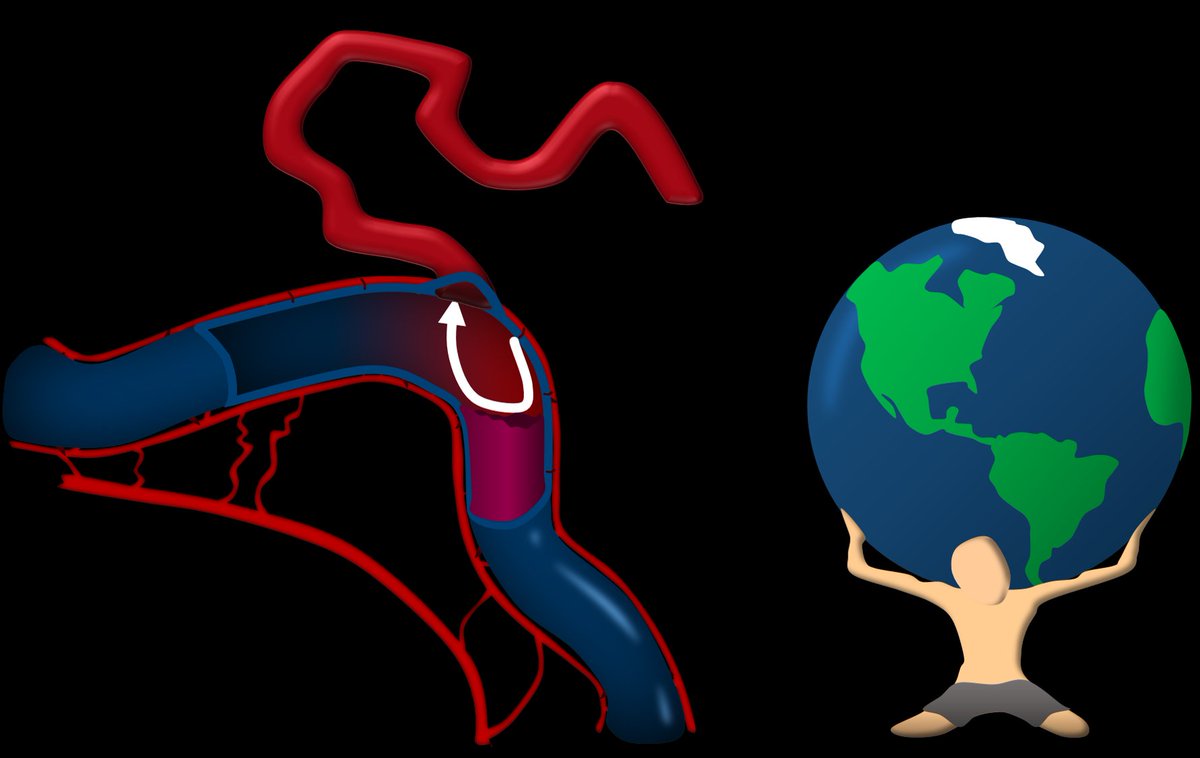
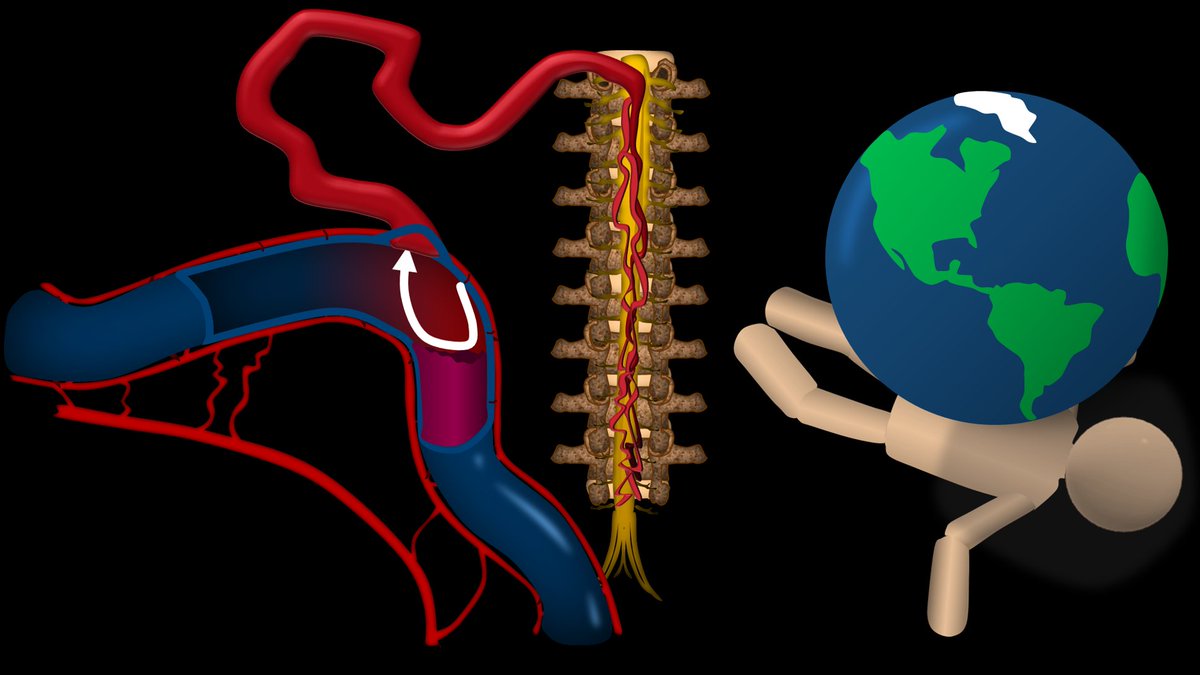
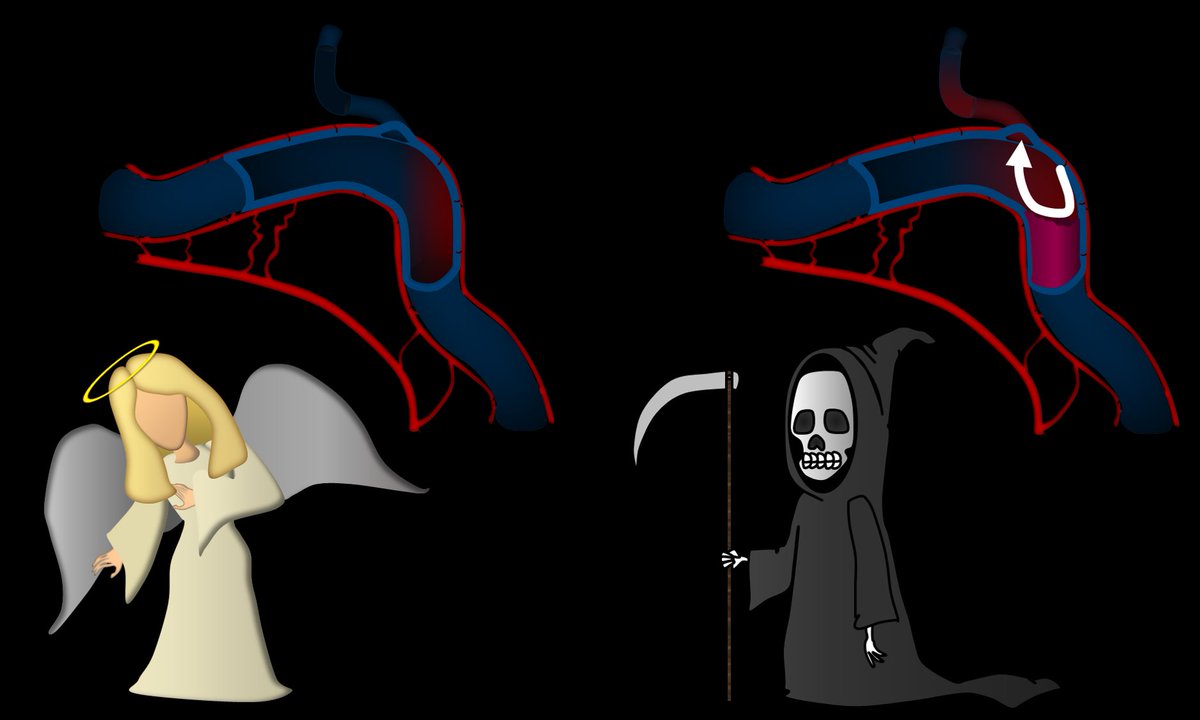
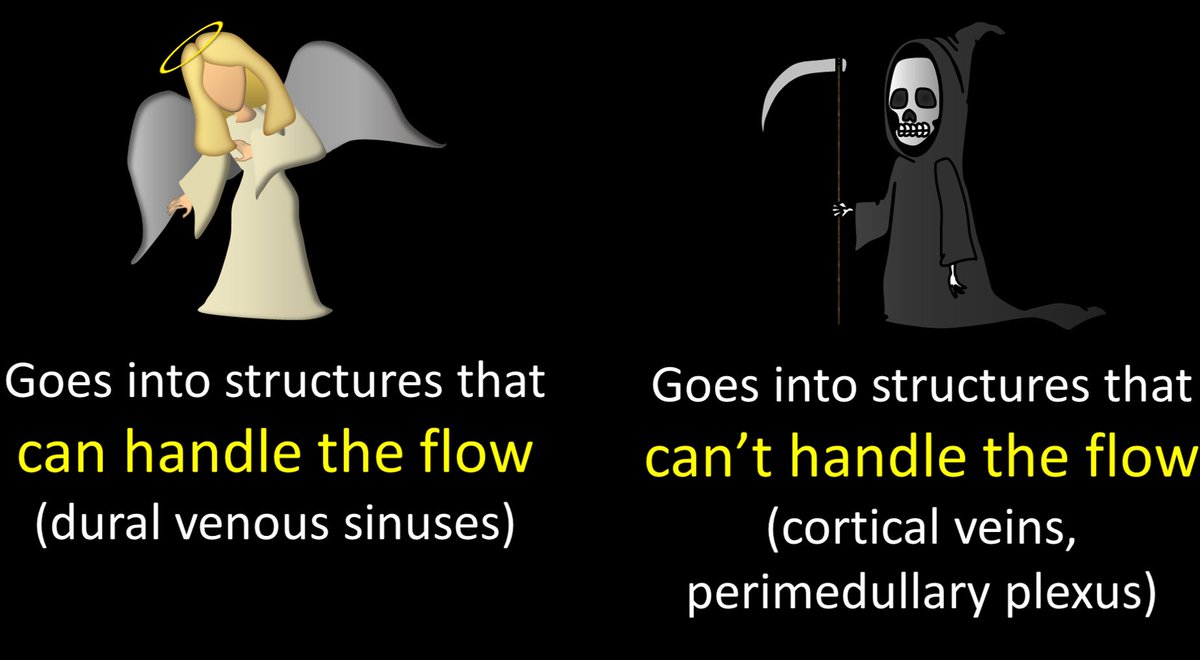
1/ Talk about dangerous liaisons! Abnormal brain vascular connections can be dangerous
A #tweetorial about an important abnormal connection: dural arteriovenous fistulas (dural AVF) in collaboration w/ @SVINJournal!
Featuring this 🆓#openaccess article: ahajournals.org
A #tweetorial about an important abnormal connection: dural arteriovenous fistulas (dural AVF) in collaboration w/ @SVINJournal!
Featuring this 🆓#openaccess article: ahajournals.org
16/
Be sure to check out the excellent review by Bradley A Gross on dAVFs featured in @SVINJournal: ahajournals.org
It’s free and open access to all!
#medtwitter #FOAMed #FOAMrad #neurorad #radres #neurosurgery
Be sure to check out the excellent review by Bradley A Gross on dAVFs featured in @SVINJournal: ahajournals.org
It’s free and open access to all!
#medtwitter #FOAMed #FOAMrad #neurorad #radres #neurosurgery
Loading suggestions...