1) Welcome to a new #accredited #tweetorial on Clinical and Laboratory Manifestations of #DKD in #T2D: From Early Identification to Monitoring Management. Your expert author is @edgarvlermamd.
2a) This activity is supported by an independent educational grant from the Boehringer Ingelheim/Lilly Alliance and is intended for healthcare providers. It is accredited for #physicians #physicianassistants #nurses #NPs #pharmacists. Check out @cardiomet_ce for more🆓CE/#CME.
2b) Past programs are still eligible for credit & can be found at cardiometabolic-ce.com. Faculty disclosures are at cardiometabolic-ce.com.
#FOAMed #medtwitter #diabetesmanagement #kidneydisease #diabetickidneydisease #diabetes @goKDIGO @MedTweetorials @nephondemand
#FOAMed #medtwitter #diabetesmanagement #kidneydisease #diabetickidneydisease #diabetes @goKDIGO @MedTweetorials @nephondemand
3) So let's talk #histmed. Symptoms of #diabetes were recorded as far back as 400 BC.
Sushruta, an Indian physician described diabetes in an ancient Hindi document as “madhumeha” or the honeyed-urine disease.
🔓satyawahr.com
🔓pubmed.ncbi.nlm.nih.gov
Sushruta, an Indian physician described diabetes in an ancient Hindi document as “madhumeha” or the honeyed-urine disease.
🔓satyawahr.com
🔓pubmed.ncbi.nlm.nih.gov
4) Around 150 AD, the Greek physician Aretaeus of Cappadocia (attention #histmed geeks, see 🔓pubmed.ncbi.nlm.nih.gov) wrote this about diabetes:
5) As to modern epidemiology, the increasing prevalence of DKD (also referred to as diabetic #nephropathy) parallels the dramatic worldwide rise in prevalence of diabetes. In 2016, estimates of diagnosed diabetes prevalence varied across US counties, ranging from 1.5% to 33.0%.
6) The median county-level prevalence of diagnosed diabetes ↗️↗️ from 7.8% in 2004 to 13.1% in 2016.
cdc.gov
cdc.gov
7) Diabetes is the number one cause of kidney failure in the US.
It is responsible for fully 4⃣4⃣% of #KidneyDisease cases.
freseniuskidneycare.com
It is responsible for fully 4⃣4⃣% of #KidneyDisease cases.
freseniuskidneycare.com
8) The driving force behind the escalating prevalence of diabetes is the global pandemic of obesity 🔓cdc.gov
9) DKD risk factors can conceptually be classified as susceptibility factors (e.g., age, sex, race/ethnicity, family history), initiation factors (e.g., hyperglycemia, AKI), & progression factors (e.g., hypertension, dietary factors, obesity)
🔓pubmed.ncbi.nlm.nih.gov
🔓pubmed.ncbi.nlm.nih.gov
10) Two of the most prominent established risk factors are #hyperglycemia and #hypertension.
12) Note that T1D usually afflicts a younger population that do not usually initially have comorbid conditions (#hypertension, #ASCVD, #obesity, etc.) often associated with #T2D and that may independently produce #CKD.
🔓accessmedicine.mhmedical.com
🔓accessmedicine.mhmedical.com
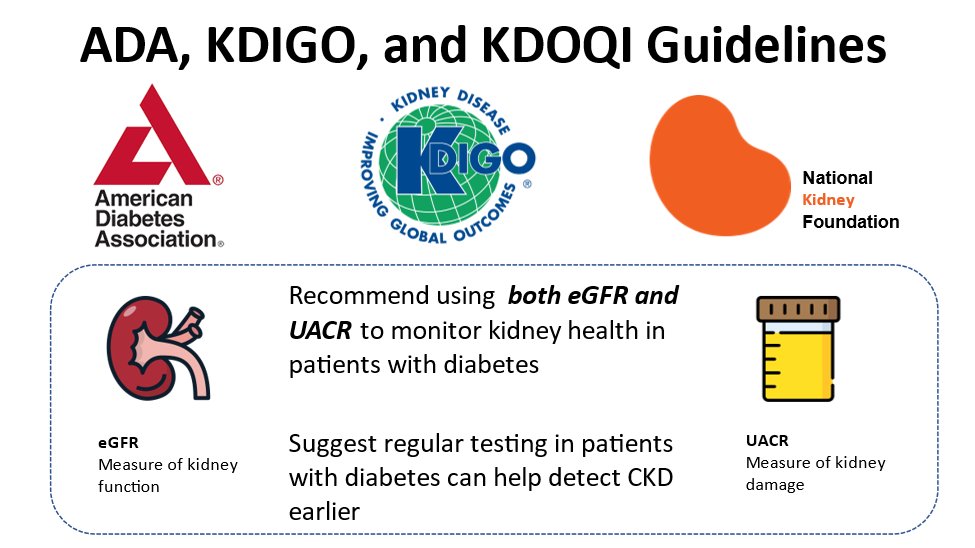
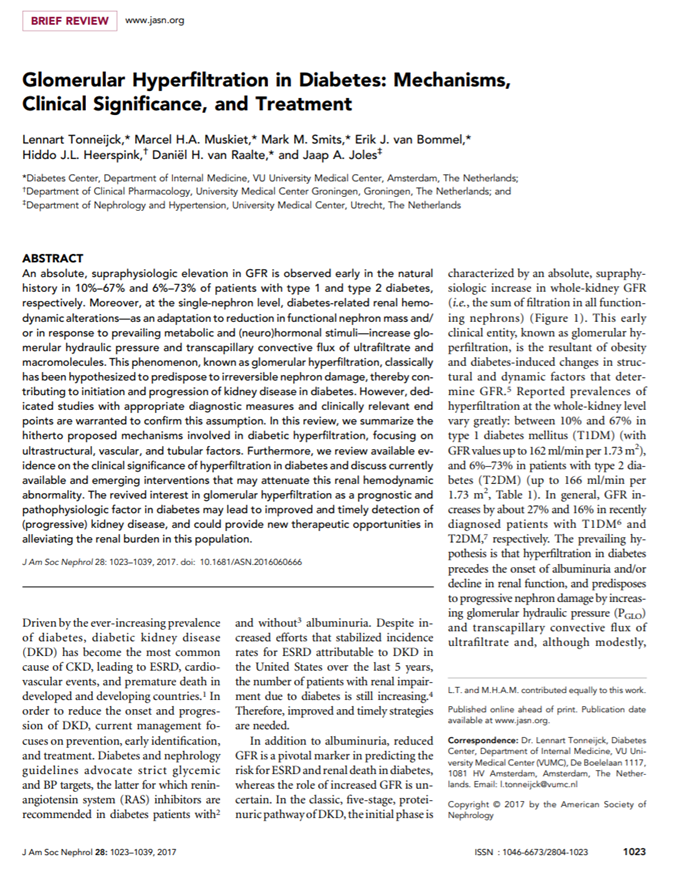
13) Patients with either T1D or T2D may exhibit an increased glomerular filtration rate (#GFR), so-called hyperfiltration, at the initial presentation of disease.
14) This hyperfiltration is mediated by proportionately greater relaxation of the afferent arteriole than the efferent arteriole and results in increased glomerular blood flow and elevated glomerular capillary pressure.
link.springer.com
link.springer.com
15) Along with this changing paradigm of the natural history of #DKD, emerging evidence suggests that the clinical presentation of DKD is altering
🔓pubmed.ncbi.nlm.nih.gov
🔓pubmed.ncbi.nlm.nih.gov
16) Let's talk🥼pathology. An early finding in patients with poorly controlled diabetes is enlargement of the kidneys, which represents predominantly hypertrophy of the existing structures rather than growth of new #nephrons or cellular hyperplasia.
17) Commissioned by the Research Committee of @Renalpathsoc an international consensus working group has provided a pathologic classification system (combining T1D and T2D #DKD) to address the heterogeneity of DKD presentation.
18) This system included scoring of 🔬glomerular, interstitial, & vascular lesions.
DKD was divided into 4 hierarchical glomerular lesions with a separate evaluation for degrees of interstitial and vascular involvement.
🔓pubmed.ncbi.nlm.nih.gov
DKD was divided into 4 hierarchical glomerular lesions with a separate evaluation for degrees of interstitial and vascular involvement.
🔓pubmed.ncbi.nlm.nih.gov
19) Renal #biopsy at the time of onset of #microalbuminuria indicates glomerular and tubular basement membrane thickening and the inception of mesangial matrix expansion.
🔓pubmed.ncbi.nlm.nih.gov
🔓pubmed.ncbi.nlm.nih.gov
20) Renal biopsy in patients who develop overt #proteinuria reveals diffuse or nodular (Kimmelstiel–Wilson) #glomerulosclerosis.
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
21) Although the Kimmelstiel–Wilson lesion is considered pathognomonic of advanced diabetic nephropathy, only approximately 25% of patients manifest this lesion.
link.springer.com
link.springer.com
23) Mark your response and return TOMORROW for the correct answer and more #accredited education!
@KIReports @NIDDKgov @ErinMichos @KatherineTuttl8 @polska_md @nephondemand @dguerrot
And in case you missed it, here's a good patient ed video for DKD: youtu.be
@KIReports @NIDDKgov @ErinMichos @KatherineTuttl8 @polska_md @nephondemand @dguerrot
And in case you missed it, here's a good patient ed video for DKD: youtu.be
24a) Welcome back! Expert author @edgarvlermamd is providing foundational knowledge on the evaluation & staging of #CKD in patients with #T2D. And YOU are earning CE/#CME! Nods to @GoggleDocs @LangoteAmit @divyaa24 @ChristosArgyrop @mvaduganathan @AgarwalRajivMD @VelezNephHepato
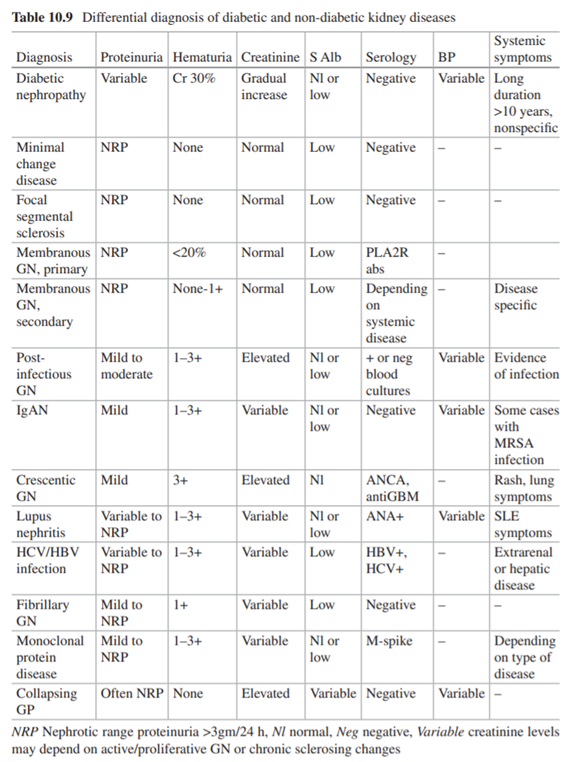
25) A nodular pattern of glomerulopathy mimicking Kimmelstiel-Wilson lesions may also be seen in light chain nephropathy. Historic descriptions of “diabetic nephropathy without overt hyperglycemia” based solely on light microscopy actually may have been light-chain disease.
26) Nodular glomerular lesions can also be observed in amyloidosis and membranoproliferative glomerulonephritis type 2.
🔓pubmed.ncbi.nlm.nih.gov
🔓pubmed.ncbi.nlm.nih.gov
27) #Microalbuminuria is more likely in patients who also have evidence of other microvascular insults, especially proliferative #retinopathy
link.springer.com
link.springer.com
28) The earliest clinical sign of the development of #DKD is usually the onset of microalbuminuria.
link.springer.com
link.springer.com
29) Initially, transient or intermittent microalbuminuria can be measured by radioimmunoassay, enzyme-linked immunosorbent assay, or special dipsticks, especially when induced by stress, physical exertion, concurrent illness, or poor glycemic control.
30) Albuminuria is a dynamic, fluctuating condition rather than a linearly progressive process.
31) So let's move now to pathobiology. Critical metabolic changes that alter kidney hemodynamics and promote inflammation and fibrosis in early diabetes include hyperaminoacidemia, a promoter of glomerular hyperfiltration and hyperperfusion, and #hyperglycemia.
32) Hyperglycemia & its metabolic sequelae are considered to be the proximate causative factor in development of diabetic #nephropathy. Hyperglycemia can induce numerous metabolic & structural abnormalities implicated in the pathogenesis of diabetic nephropathy, including ...
33) ..generation of reactive oxygen species, activation of the polyol pathway (leading to de novo synthesis of diacylglycerol & increased protein kinase C activity), alterations in the hexosamine pathway, & nonenzymatic protein glycation (advanced glycosylation end products).
34) Although experimental studies have indicated that each of these alterations can be causative in animal models of diabetic nephropathy, their role in human diabetic nephropathy remains incompletely determined.
35) Better glucose control does generally reduce the risk of nephropathy and other microvascular complications, especially in type 1 diabetes
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
36) What about renal #hemodynamics? Glomerular hyperfiltration is a well characterized consequence of early diabetes. Overall, it is observed in 10%–40% or up to 75% of patients with #T1D and up to 40% of patients with #T2D.
37) In T2D, systemic #hypertension and #obesity also contribute to glomerular hyperfiltration via various mechanisms, such as high transmitted systemic BP and glomerular enlargement.
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
38) Mechanisms underlying glomerular hyperfiltration in diabetes are incompletely understood; one plausible mechanism is⬆️proximal tubular reabsorption of glucose via #SGLT2, which⬇️distal delivery of solutes, particularly NaCl, to the macula densa.
🔓pubmed.ncbi.nlm.nih.gov
🔓pubmed.ncbi.nlm.nih.gov
39) The resulting⬇️in tubuloglomerular feedback may dilate the afferent arteriole to⬆️glomerular perfusion, while concurrently, high local production of angiotensin II at the efferent arteriole produces vasoconstriction.
40) The overall effect is high intraglomerular pressure and glomerular hyperfiltration.
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
41) There's even more to the #pathophysiology of #DKD: #DM causes overactivation of the mineralocorticoid receptor, which⬆️the expression of proinflammatory cytokines & profibrotic proteins, leading to inflammation & fibrosis.
🔓pubmed.ncbi.nlm.nih.gov
🔓pubmed.ncbi.nlm.nih.gov
42) So what about screening for diagnosing #DKD? Screening should be performed annually for patients with #T1D beginning 5 years after diagnosis and annually for all patients with #T2D beginning at the time of diagnosis.
link.springer.com
link.springer.com
43) So re making that diagnosis, mark your choice below and return tomorrow for the correct answer, the rest of the education in this #tweetorial, and your CE/#CME credit grab!
The diagnosis of DKD requires which of the following?
The diagnosis of DKD requires which of the following?
44) Welcome back! You are but a few 🖱️clicks away from free CE/#CME as @edgarvlermamd teaches us about the pathophysiology and lab assessment of diabetic #KidneyDisease #DKD. Join the fun and follow us! You'll also find great #tweetorials from @edgarvlermamd on @ckd_ce!
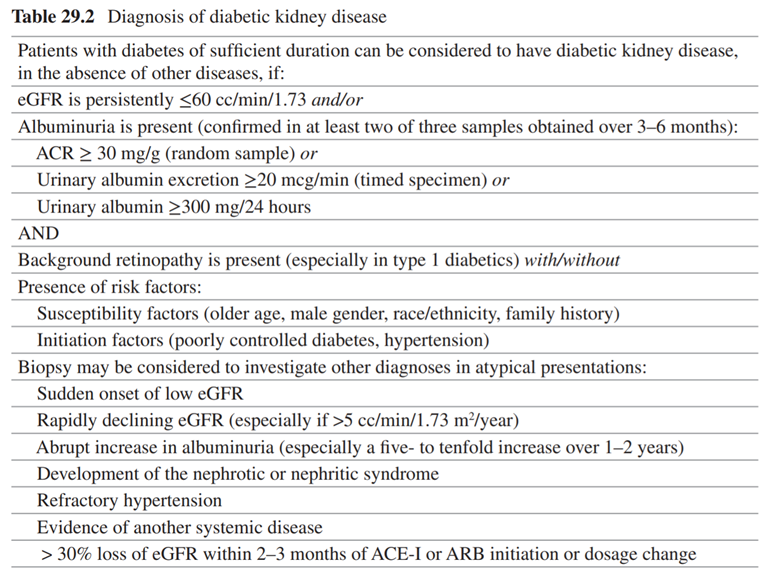
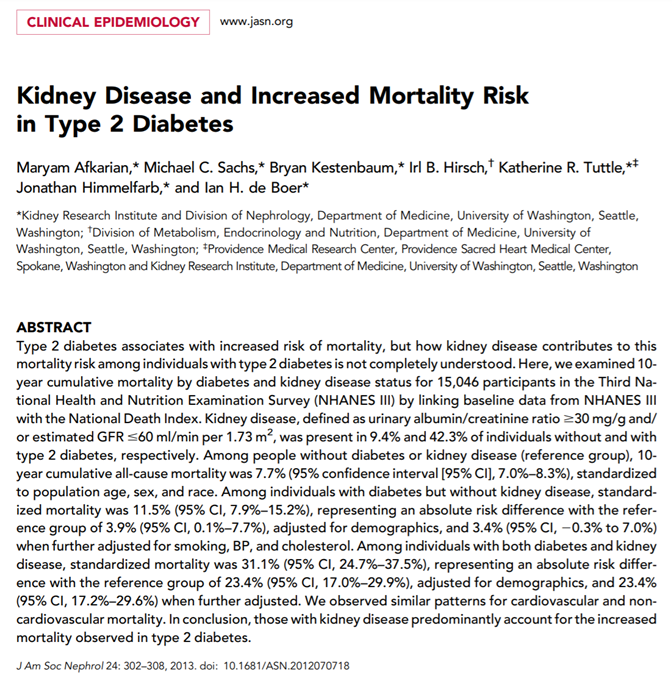
45) The clinical diagnosis of DKD is on the basis of measurement of #eGFR and #albuminuria along with clinical features, such as diabetes duration and presence of diabetic #retinopathy.
link.springer.com
link.springer.com
47) The preferred test for albuminuria is a urinary albumin-to-creatinine ratio (UACR) performed on a spot sample, preferably in the morning.
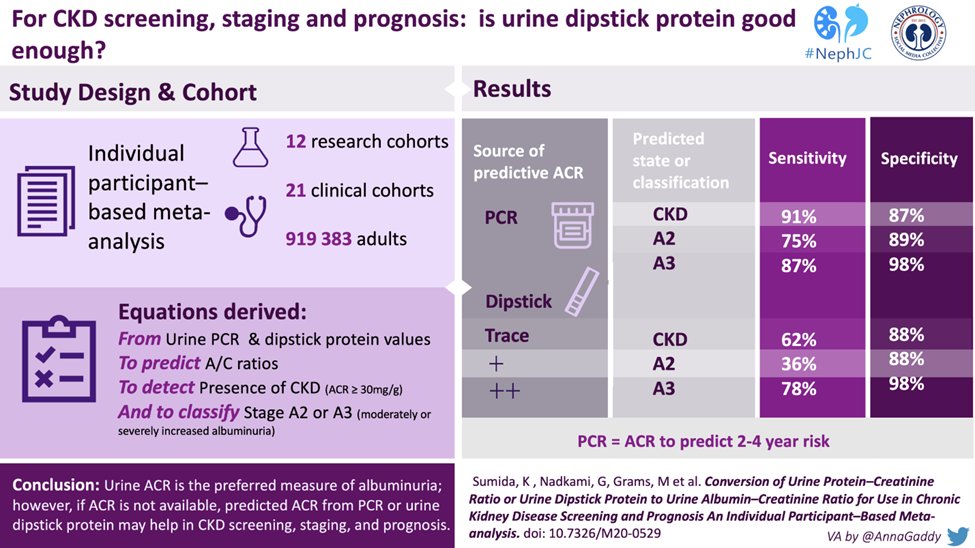
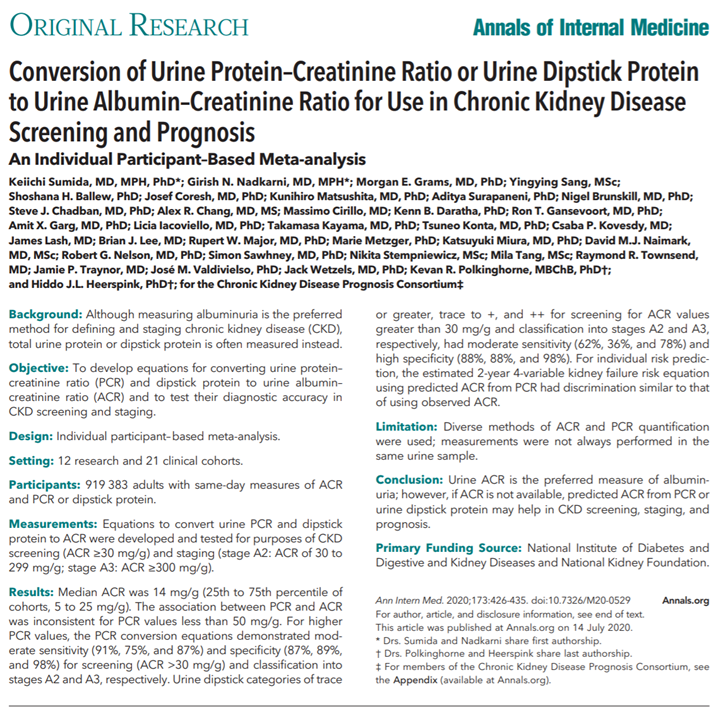
48) This study showed that if UACR is not available, predicted UACR from UPCR or urine dipstick protein may help in CKD screening, staging, and prognosis.
#VisualAbstract by @AnnaGaddy
🔓pubmed.ncbi.nlm.nih.gov
#VisualAbstract by @AnnaGaddy
🔓pubmed.ncbi.nlm.nih.gov
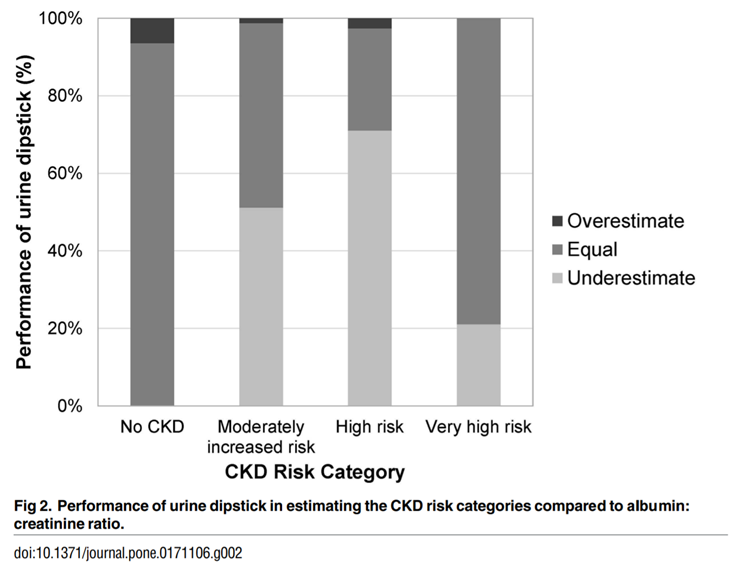
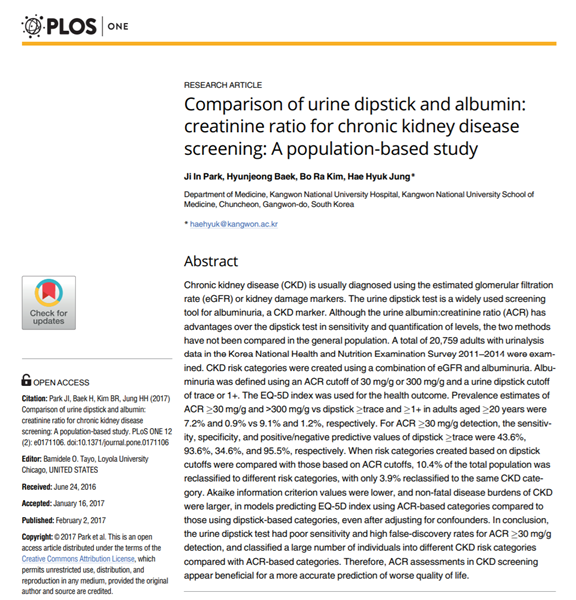
49) Urine dipstick underestimates CKD risk as compared with UACR.
Data from an analysis of the Korean NHANES 2011-2014 among adults at least 20 years of age with available urinalysis data (n=20,759).
Data from an analysis of the Korean NHANES 2011-2014 among adults at least 20 years of age with available urinalysis data (n=20,759).
50) Over ½ of patients in the moderately increased and high-risk categories were classified into lower-risk categories using the dipstick test
🔓pubmed.ncbi.nlm.nih.gov
🔓pubmed.ncbi.nlm.nih.gov
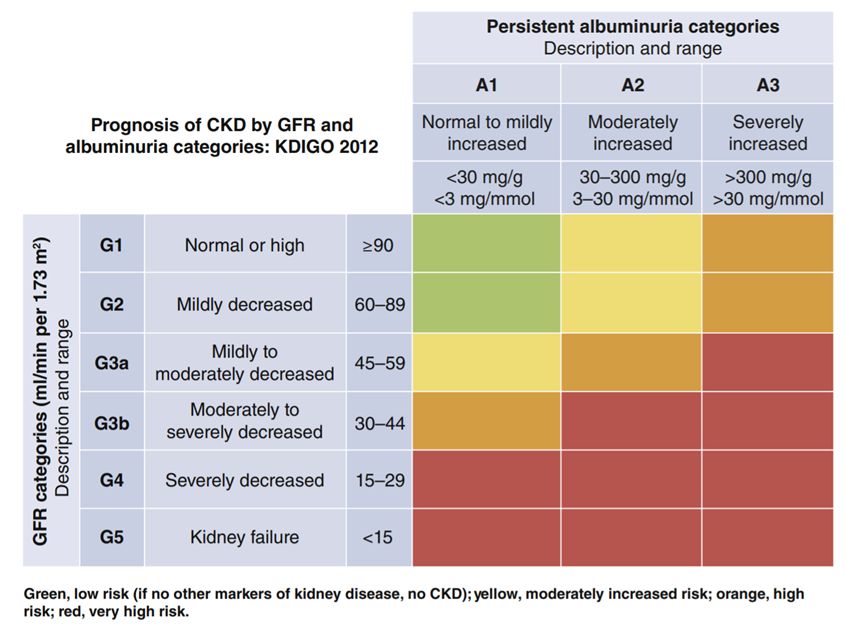
51) DKD is identified clinically by persistently high UACR ≥30 mg/g and/or sustained reduction in eGFR <60 ml/min per 1.73 m2. See @goKDIGO
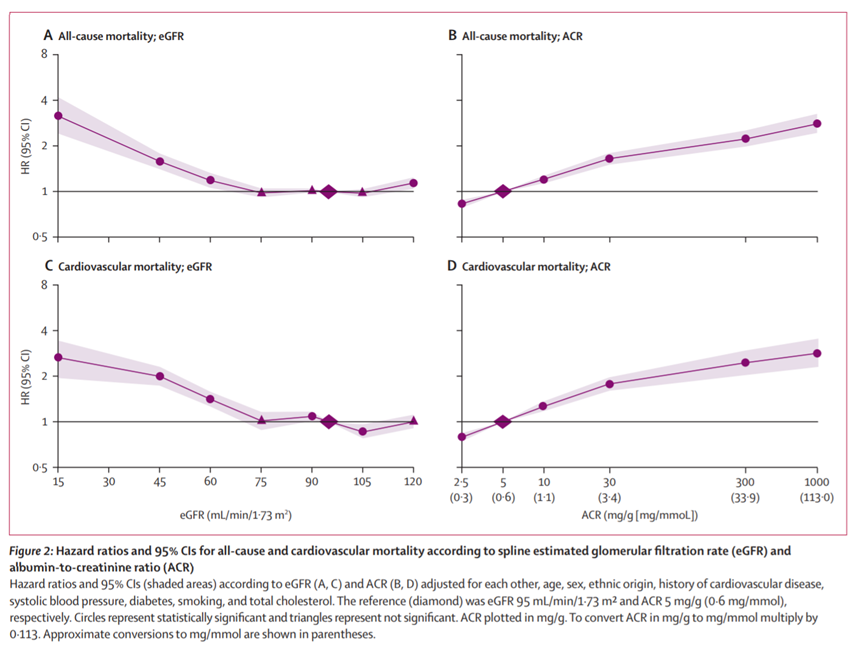
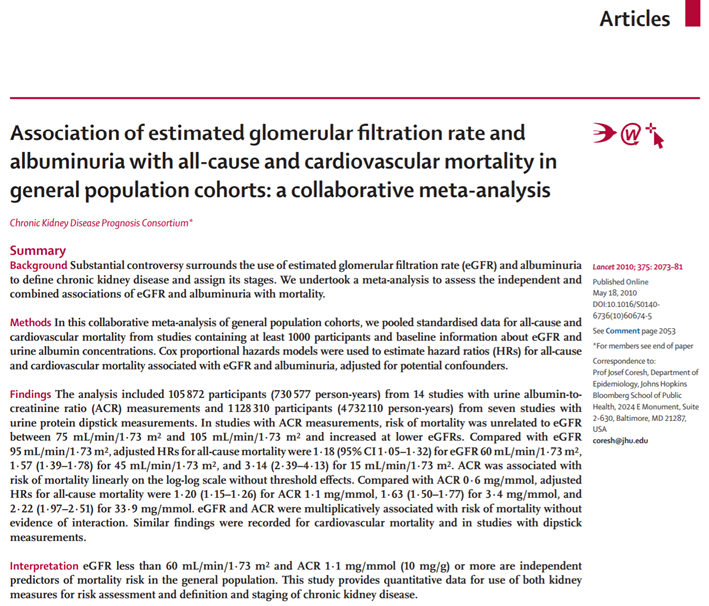
52) A meta-analysis of 21 general population cohort studies (n=1,234,182; median follow-up of 7.9yr) found UACR ≥10 mg/g & eGFR <60 mL/min/1.73 m2 were significantly associated with an increased risk of CV mortality, independently of each other and of traditional risk factors.
53) The mortality gradient conferred by higher albuminuria within all but the lowest eGFR category was > 2x.
This was > the risk between adjacent CKD stages based on eGFR, suggesting that albuminuria provides > prognostic information beyond eGFR.
🔓pubmed.ncbi.nlm.nih.gov
This was > the risk between adjacent CKD stages based on eGFR, suggesting that albuminuria provides > prognostic information beyond eGFR.
🔓pubmed.ncbi.nlm.nih.gov
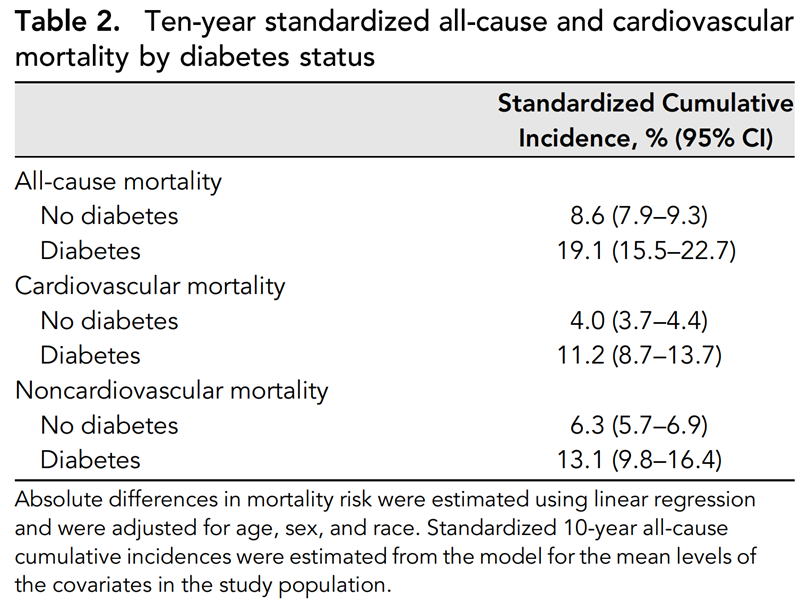
54) 3rd #NHANES (n=15,046) showed those w/CKD+T2D were at⬆️risk of 10y CV mortality, comp to T2D alone.
Patients /CKD+T2D are 3x more likely to die of CV causes than with T2D alone.
CKD+T2D also⬆️risk of 10y all-cause mortality vs either alone.
🔓jasn.asnjournals.org
Patients /CKD+T2D are 3x more likely to die of CV causes than with T2D alone.
CKD+T2D also⬆️risk of 10y all-cause mortality vs either alone.
🔓jasn.asnjournals.org
56) Albuminuria onset occurs sooner than a decline in GFR to levels <60 mL/min/1.73 m2, which may allow for earlier management of CKD progression.
🔓pubmed.ncbi.nlm.nih.gov
🔓pubmed.ncbi.nlm.nih.gov
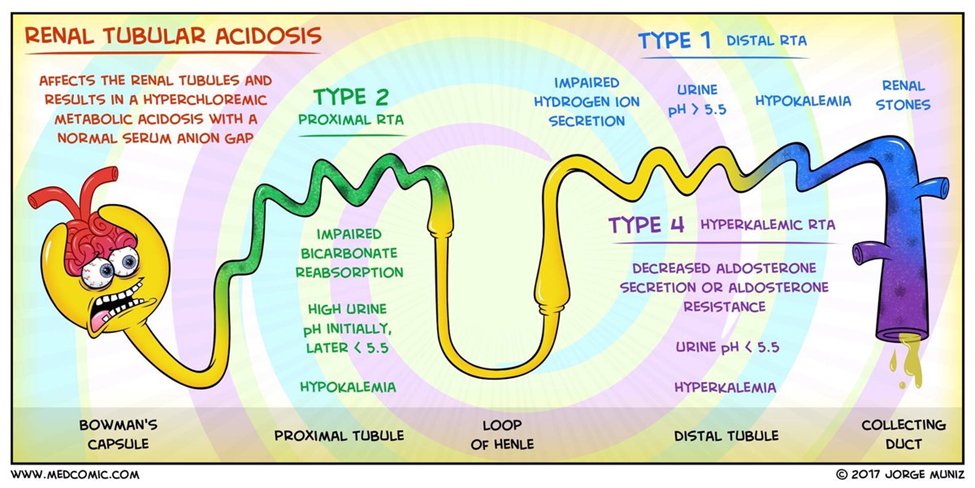
57) Patients with diabetes also experience an increased rate of other kidney abnormalities.
Type 4 (hyporeninemic, hypoaldosteronemic) metabolic acidosis with hyperkalemia is commonly encountered in patients with diabetes and mild to moderate renal insufficiency.
Type 4 (hyporeninemic, hypoaldosteronemic) metabolic acidosis with hyperkalemia is commonly encountered in patients with diabetes and mild to moderate renal insufficiency.
58) These patients should be carefully monitored for the development of hyperkalemia in response to volume depletion or after the initiation of drugs that interfere with the renin angiotensin system, such as ACE inhibitors and ARBs.
Artwork by @medcomic
Artwork by @medcomic
59) If features atypical of DKD are present, then other causes of kidney disease should be considered. link.springer.com
60) Atypical features include
- sudden onset of low eGFR or rapidly⬇️ing eGFR
- abrupt⬆️in albuminuria or development of nephrotic or nephritic syndrome
- refractory #hypertension
-signs/sx of another systemic disease
- >30% eGFR ⬇️within 2–3mo of initiation of a #RAASi
- sudden onset of low eGFR or rapidly⬇️ing eGFR
- abrupt⬆️in albuminuria or development of nephrotic or nephritic syndrome
- refractory #hypertension
-signs/sx of another systemic disease
- >30% eGFR ⬇️within 2–3mo of initiation of a #RAASi
61) And now you have made it! 🆓 CE/#CME! #Physicians #pharmacists #nurses #PAs: go to cardiometabolic-ce.com and claim your credit! I am @edgarvlermamd. Follow @cardiomet_ce (& @ckd_ce) for more #tweetorials! #medtwittter #cardiotwitter #diabetickidneydisease #nephtwitter
Loading suggestions...