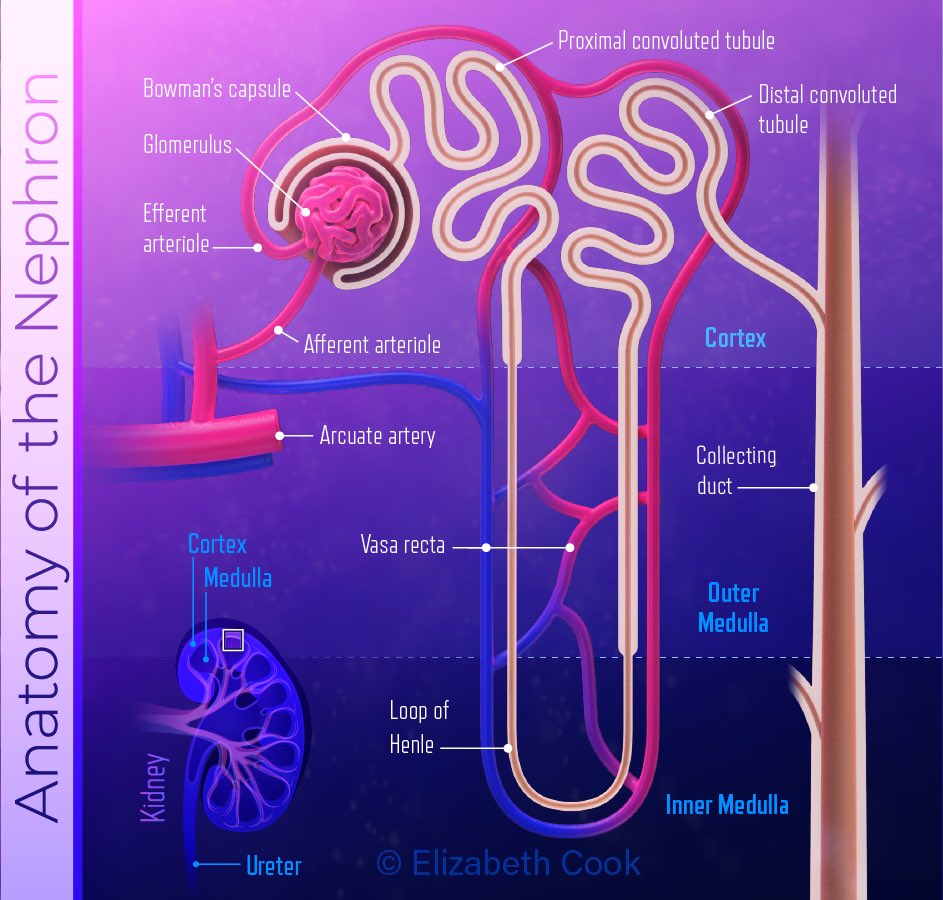
Intrarenal or sometimes called intrinsic acute kidney injury happens when damage to the kidneys tubules like glomerulus, interstitium, causes a sudden loss in kidney function.
The most common cause of Intrarenal Acute Kidney injury is
Acute Tubular Necrosis (ATN)
Which is a condition in where the small filtering tubes in the kidney are injured (epithelial cells die due to ischemia)
Picture’s from: researchgate.net
Acute Tubular Necrosis (ATN)
Which is a condition in where the small filtering tubes in the kidney are injured (epithelial cells die due to ischemia)
Picture’s from: researchgate.net
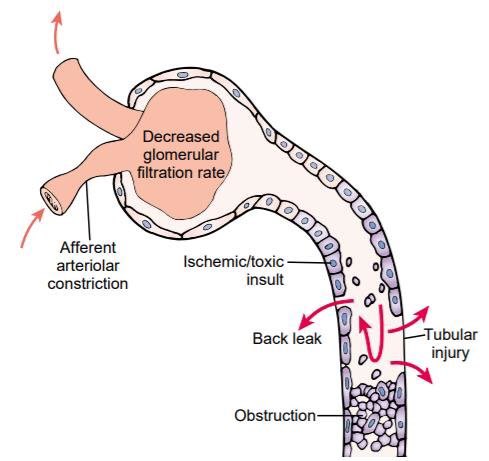
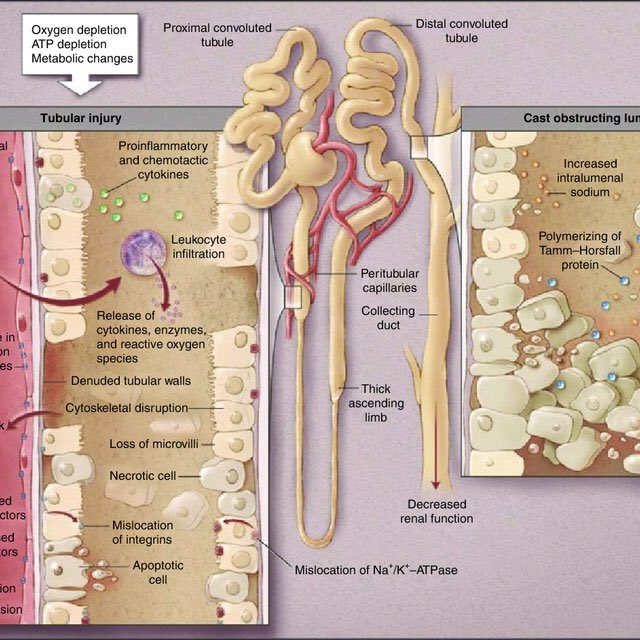
What happens?
proximal tubular cells fall into the tubular lumen→debris build up & obstruct tubules→leads to High pressure tubules → blood moves from high p blood vessels to high pressure tubles→ decrease blood filtered→ decreased GFR
Picture from: researchgate.net
proximal tubular cells fall into the tubular lumen→debris build up & obstruct tubules→leads to High pressure tubules → blood moves from high p blood vessels to high pressure tubles→ decrease blood filtered→ decreased GFR
Picture from: researchgate.net
This this will lead to decreased urine output👉🏼Oliguria
Urea and creatinine will not be filtered properly👉🏼increase retention of them in blood👉🏼 azotemia
Since the cells are ischemic can’t filter blood, eventually it’ll lead to Hyperkalemia, metabolic acidosis and uraemia ☹️
Urea and creatinine will not be filtered properly👉🏼increase retention of them in blood👉🏼 azotemia
Since the cells are ischemic can’t filter blood, eventually it’ll lead to Hyperkalemia, metabolic acidosis and uraemia ☹️
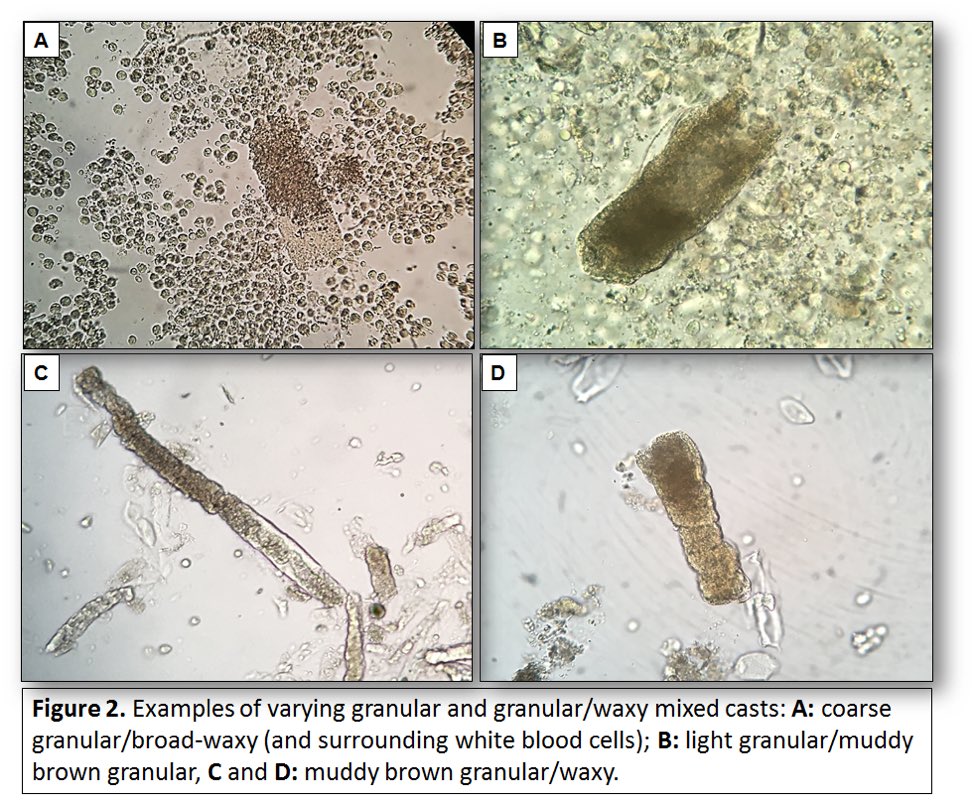
Later on, dead cells that have built in the tubules will form a brown granular caste
This brown cast will be excreted which will cause the diagnostic features of Muddy brown granular cast in urine👇🏼
Picture is from: renalfellow.org
This brown cast will be excreted which will cause the diagnostic features of Muddy brown granular cast in urine👇🏼
Picture is from: renalfellow.org
Upon the cause, the patient is managed
Some patients will experience tubular re-epithelialisation and gain full-recovery when treated adequately 😁👍🏼
Some patients will experience tubular re-epithelialisation and gain full-recovery when treated adequately 😁👍🏼
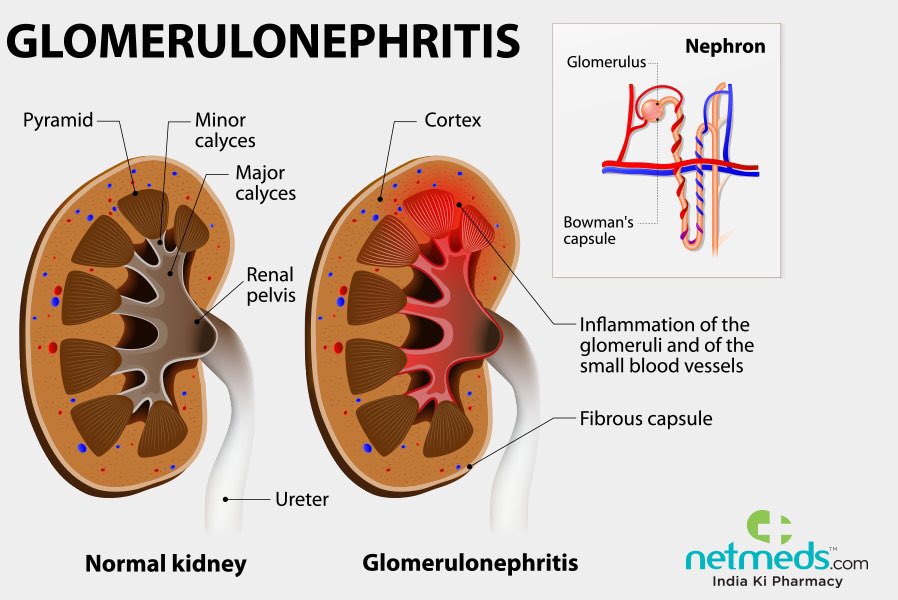
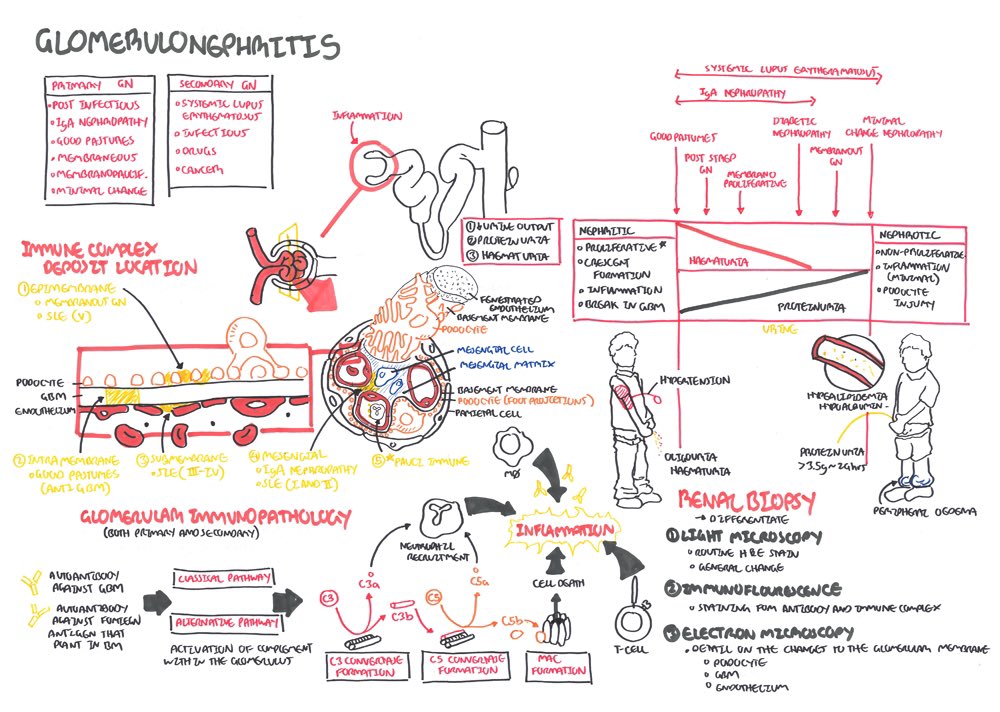
It’s usually caused by antigen-antibody complexes deposition in the glomerular tissue👉🏼activate complement system 👉🏼 lead to inflammation 😳
Quick recap!😊
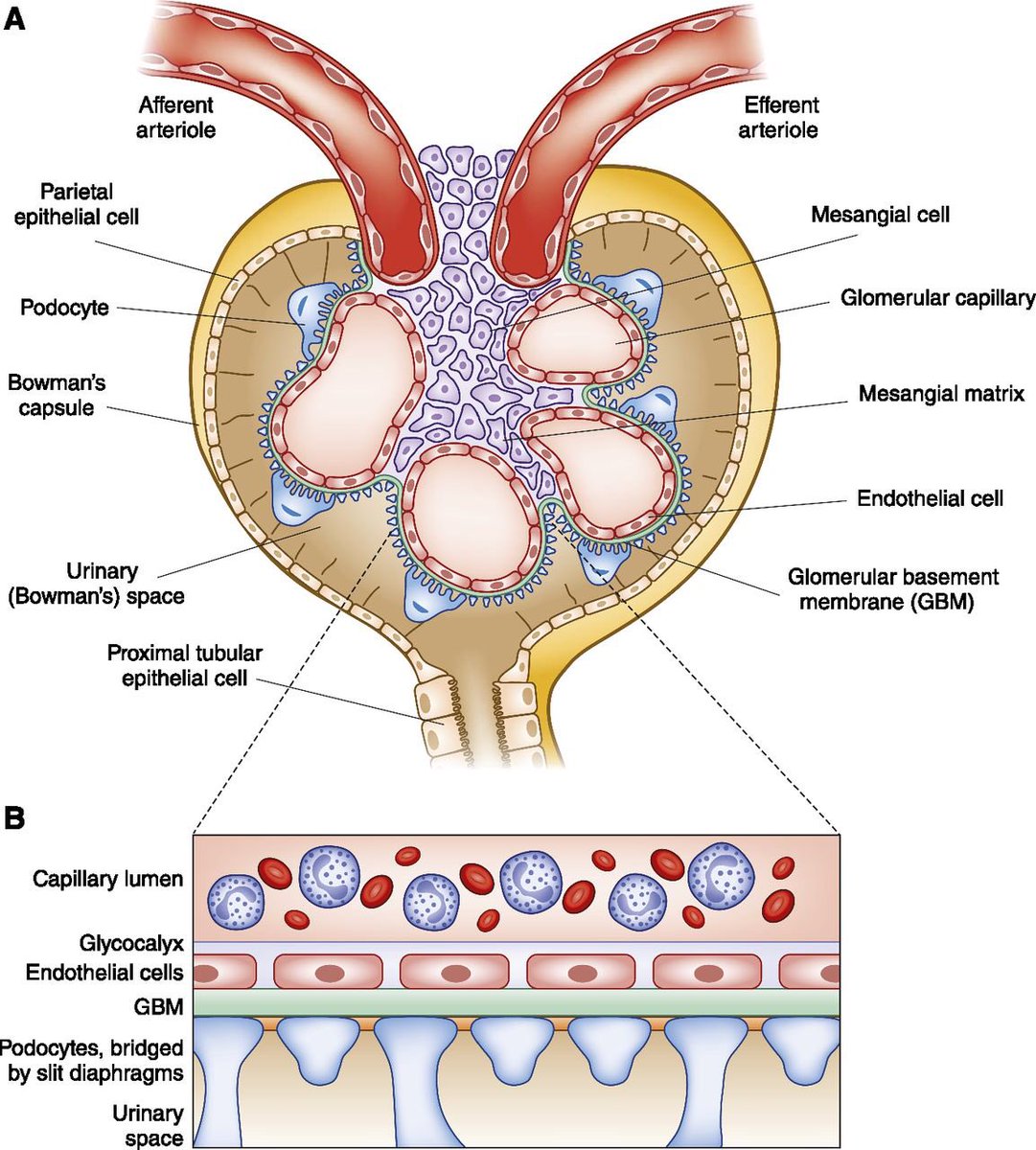
The endothelium of the fenestrated capillaries are covered with negatively charged proteoglycans & glycosaminoglycans.
Quick recap!😊
The endothelium of the fenestrated capillaries are covered with negatively charged proteoglycans & glycosaminoglycans.
The glomerular basement membrane connects the capillaries and the surrounding Bowman’s capsule thus it is also covered with proteoglycans👉🏼 negatively charged
Picture is from: cjasn.asnjournals.org
Picture is from: cjasn.asnjournals.org
The cells of the visceral layer of Bowman’s capsule are called podocytes, whose processes also form a kind of meshwork
This meshwork prevents filtration of large molecules and anions
💪🏼😤
This meshwork prevents filtration of large molecules and anions
💪🏼😤
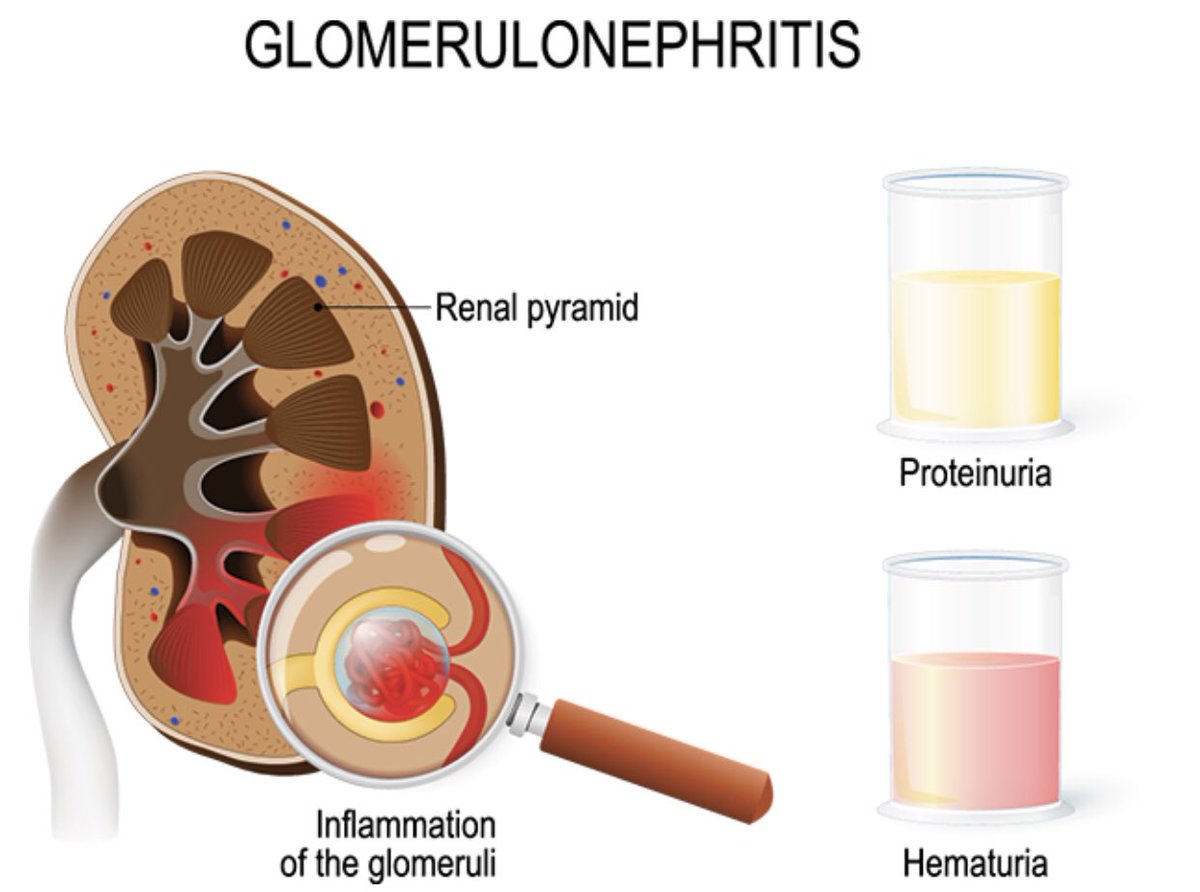
When damaged the membrane permeability ⬆️ and large molecules like protein and blood are filtered ☹️
It can cause the diagnostic features of proteinuria and hematuria
Picture is from: healthychildren.org
It can cause the diagnostic features of proteinuria and hematuria
Picture is from: healthychildren.org
Since the door is open & large molecules enter👉🏼fluid leakage will ⬇️pressure difference 👉🏼 will eventually decrease the GFR due to ongoing damage in the glomeruli
Low GFR👉🏼Low urine output
Possible increased fluid retention
👉🏼 Oedema
Picture’s from: armandoh.org
Low GFR👉🏼Low urine output
Possible increased fluid retention
👉🏼 Oedema
Picture’s from: armandoh.org
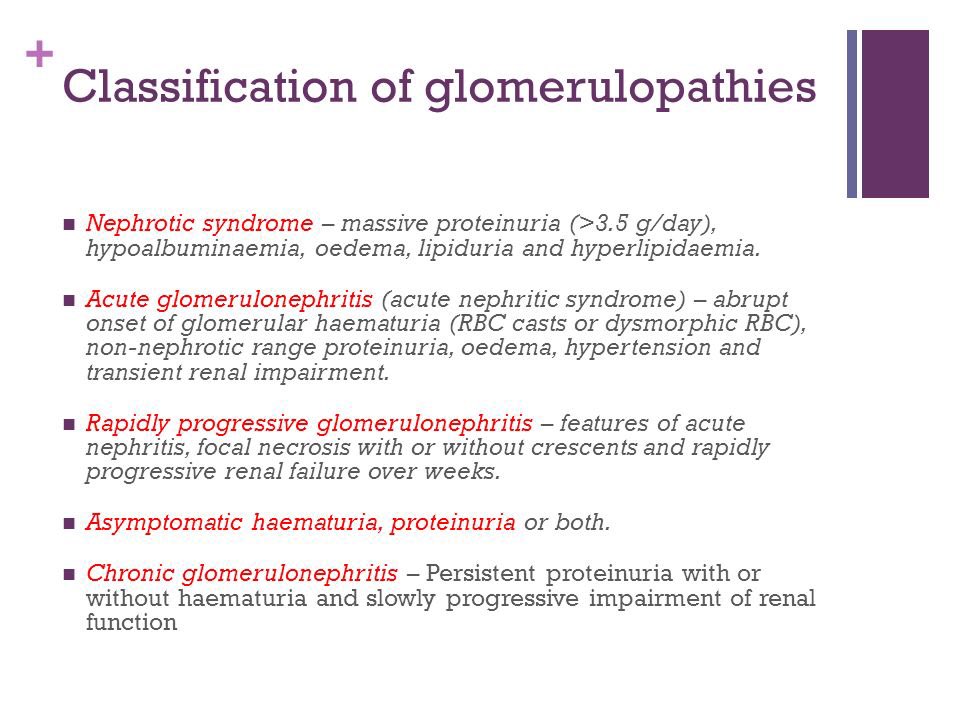
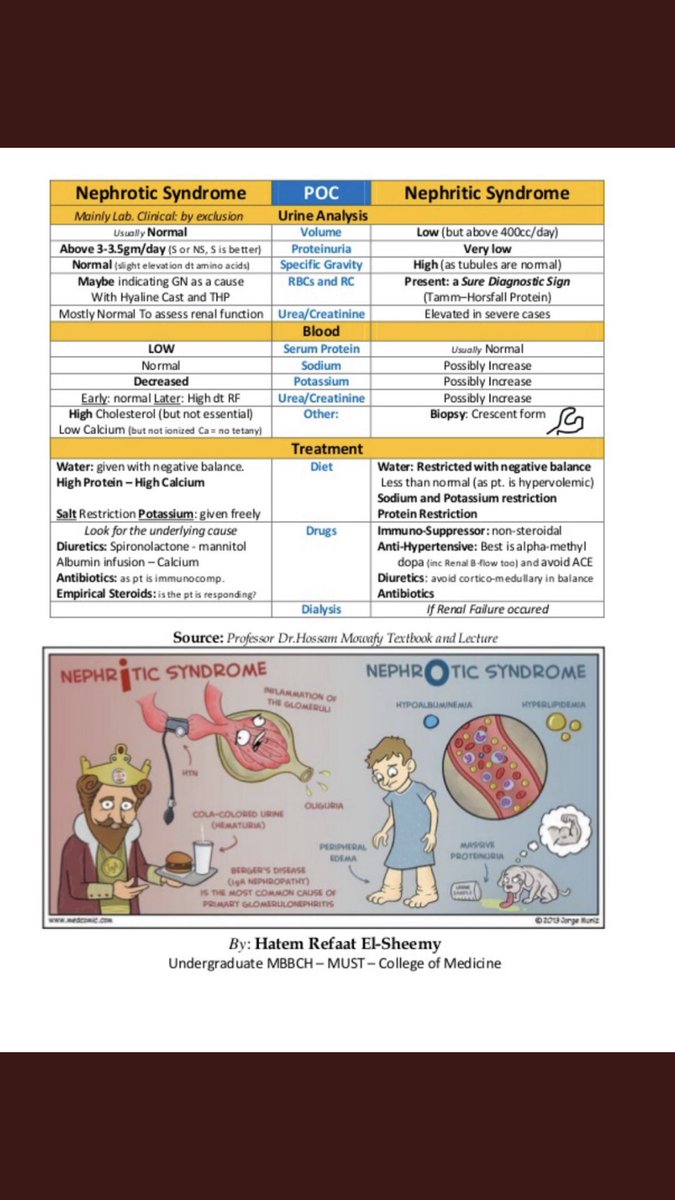
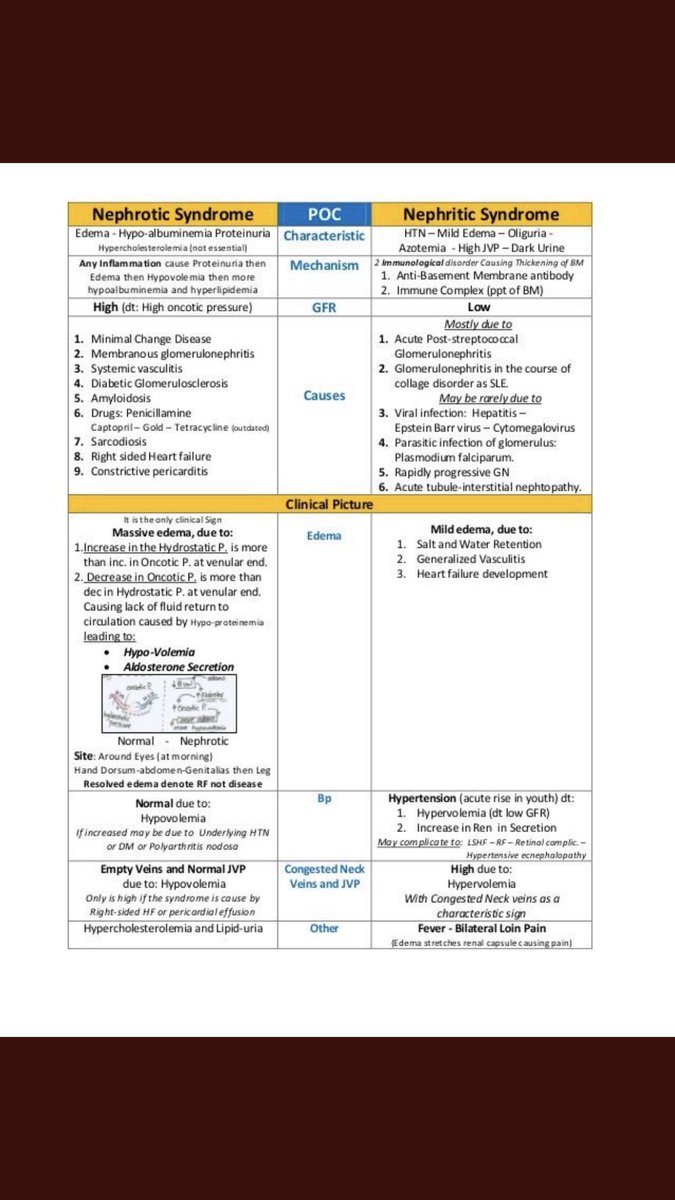
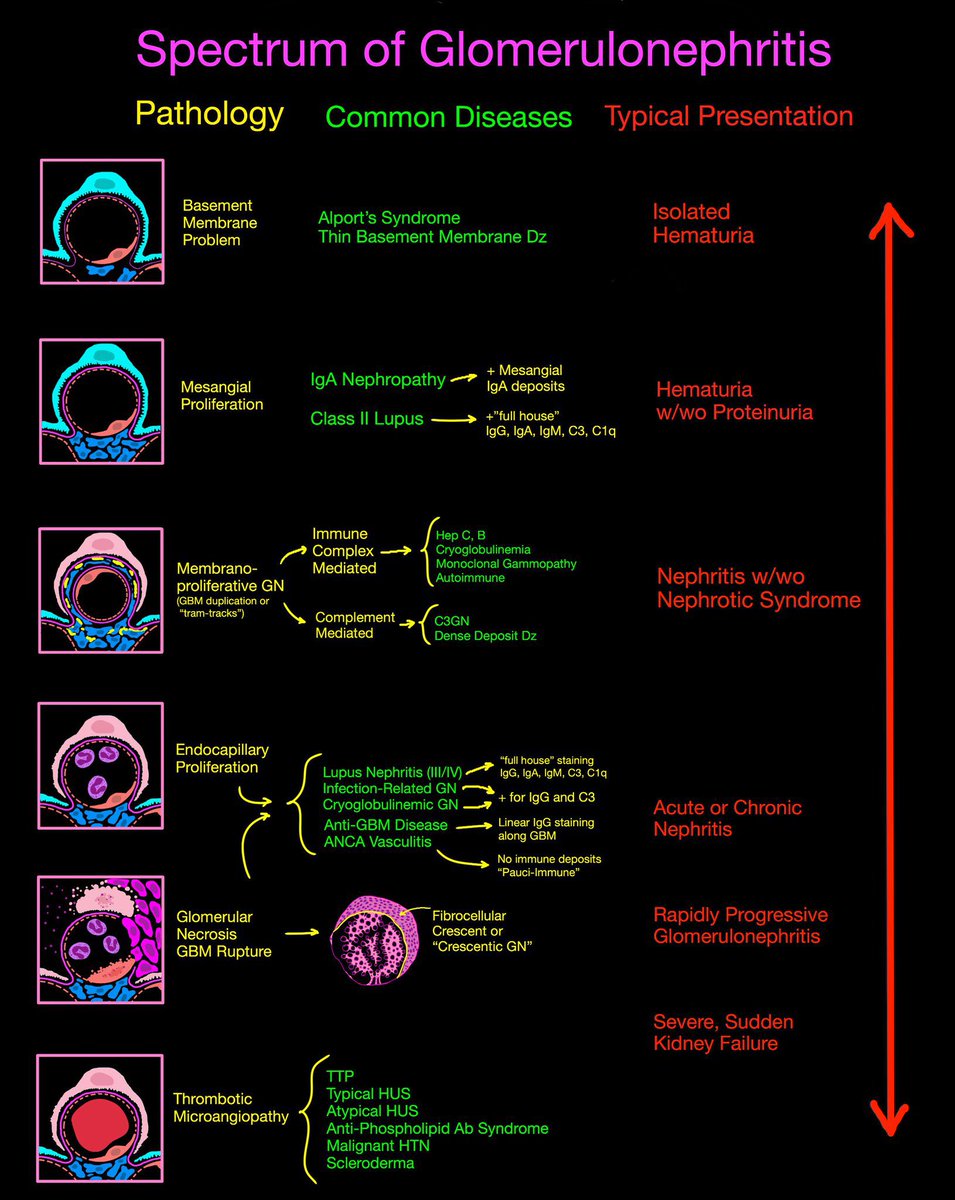
The classification of glomerulopathies and the difference between nephrotic and nephritic syndrome 👌🏼😍
Image is from: google.com
Image is from: google.com
Loading suggestions...