For the fellows, this case is the penultimate learning case for bleeding. Prepare yourself this is THE nightmare.
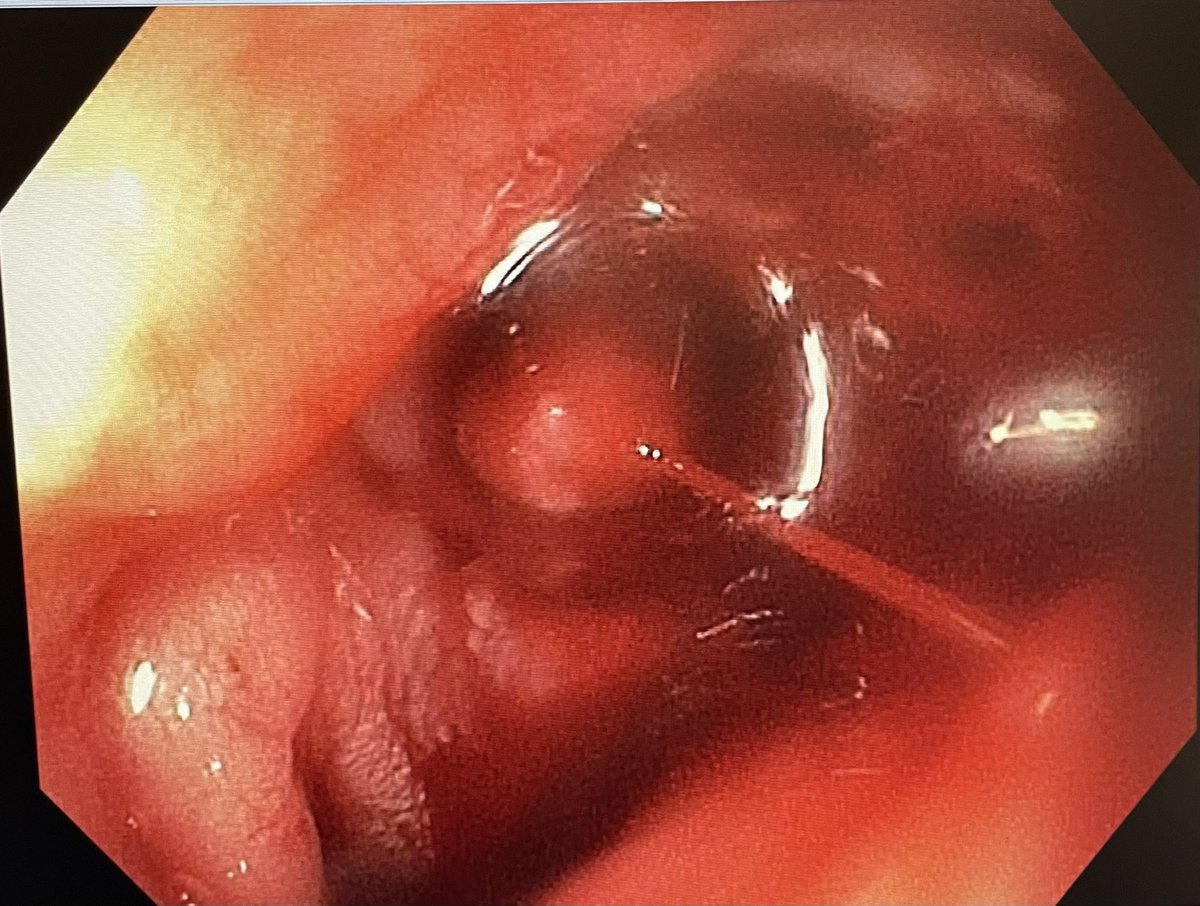
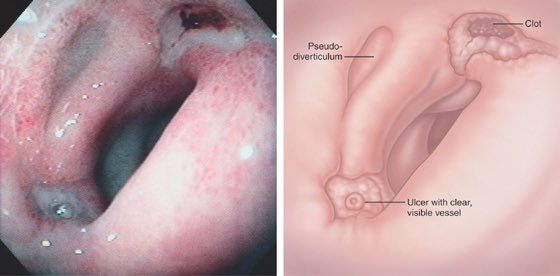
You see this duodenal ulcer with adherent clot. What you would you do next?
#GITwitter @ScopingSundays
You see this duodenal ulcer with adherent clot. What you would you do next?
#GITwitter @ScopingSundays
What do you think do next?
What do you do next?
As the bipolar probe cannot reach the target vessel, what would you do next?
The patient is destabilizing.
The patient is destabilizing.
While tamponade was held for 5 minutes…
Hemospray was prepared and multiple scopes, including duodenoscope (En fos view) and another gastroscope (preload OTSC) were brought in.
IR cleared their next case for us.
A breath was taken.
Think plan C, D as your move to plan B.
Hemospray was prepared and multiple scopes, including duodenoscope (En fos view) and another gastroscope (preload OTSC) were brought in.
IR cleared their next case for us.
A breath was taken.
Think plan C, D as your move to plan B.
The duodenoscope was attempted but quickly abandoned as the pylorus could not be crossed blind through a torrent of blood.
What’s left ?
Loading suggestions...