1) Welcome to our accredited tweetorial on optimal contemporary chronic mgt of #hyperkalemia. Earn 0.5h CME/CE credit by following this thread. I am @edgarvlermamd. @MedTweetorials #medtwitter #cardiotwitter #endotwitter #nephtwitter #nephjc @kidney_boy @DanielJDrucker
Supported by educational grants from Abbott, AstraZeneca, Bayer, Chiesi, NovoNordisk. This program is intended for healthcare providers.
2) First, a case: 67M with T2D, HTN, HFpEF is referred for CKD evaluation. Meds include Metformin, Lisinopril, Amlodipine, and Metoprolol. Pertinent Labs: Na 138, K 5.8, BUN/ Crea 32/ 2.6, A1C 7.6%.
3) Risk Factors for #hyperkalemia include: Advanced stages of #CKD, #heartfailure, resistant #hypertension, #diabetes, myocardial infarction (#MI), and/or, combinations of these conditions (pubmed.ncbi.nlm.nih.gov, pubmed.ncbi.nlm.nih.gov, pubmed.ncbi.nlm.nih.gov)

pubmed.ncbi.nlm.nih.gov/28866674/
Association of Serum Potassium with All-Cause Mortality in Patients with and without Heart Failure, Chronic Kidney Disease, and/or Diabetes - PubMed
Mortality risk progressively increased with dyskalemia and was differentially greater in those with...
pubmed.ncbi.nlm.nih.gov/27418967/
pubmed.ncbi.nlm.nih.gov/28158516/
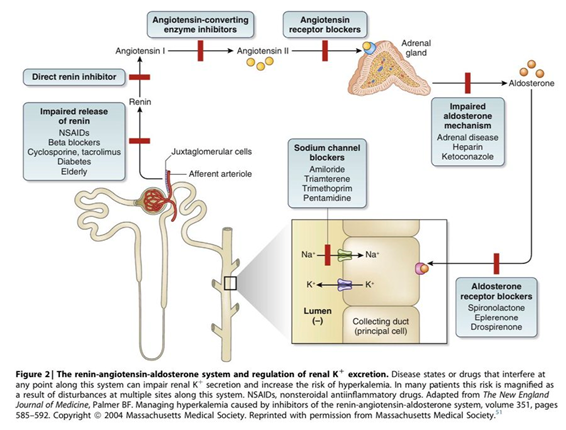
4) Additional risk factors include #RAASi usage, advanced age, and drugs such as #heparin, ẞ-blockers, nonsteroidal anti-inflammatory drugs, #calcineurin inhibitors, #trimethoprim, #pentamidine, and K-sparing diuretics.
5) The risk of hyperkalemia progressively increases as eGFR decreases <15 mL/min per 1.73 m2. See ncbi.nlm.nih.gov and pubmed.ncbi.nlm.nih.gov
6) Furthermore, patients receiving #RAASi therapy who have an eGFR < 60 mL/min per 1.73 m2 have an elevated #hyperkalemia risk, which progressively increases as eGFR decreases.
7) RAASi are recommended for patients with hypertension, HF, stable coronary artery disease, CKD, diabetic kidney disease (#DKD), and diabetes. They improve survival in patients with CKD, HF, and post-MI status and also provide kidney benefits in patients with non-DKD and DKD.
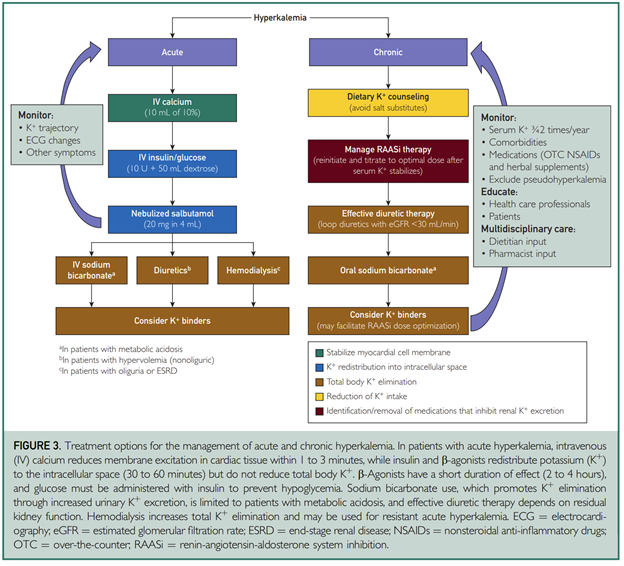
9) What are the treatment options for the management of his hyperkalemia?
A. Diet
B. Removal of other hyperkalemia-causing drugs
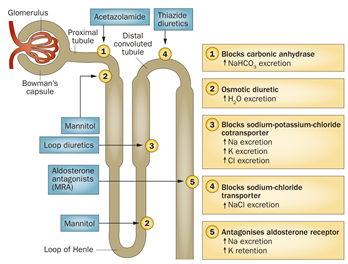
C. Use of diuretics
D. Modification of RAASi dose
E. K+ binders
A. Diet
B. Removal of other hyperkalemia-causing drugs
C. Use of diuretics
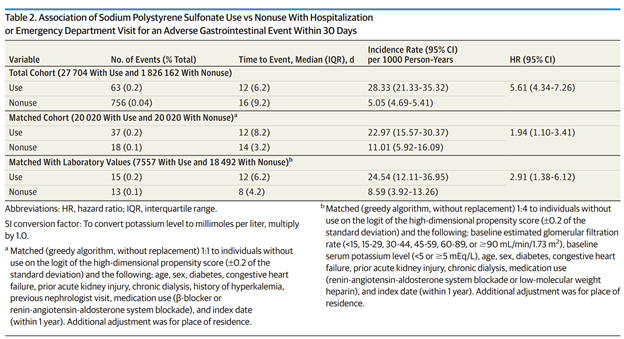
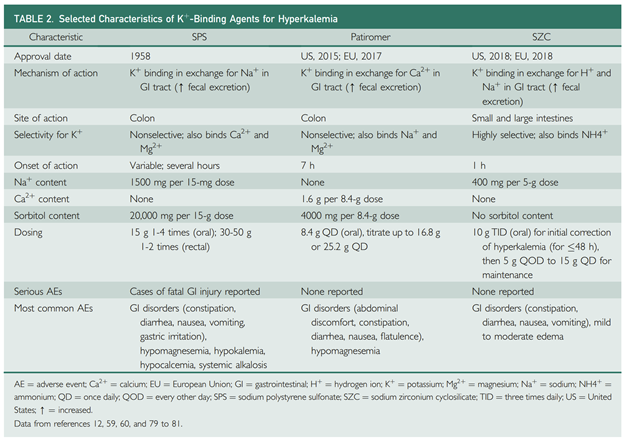
D. Modification of RAASi dose
E. K+ binders
10) Mark your answer and return tomorrow for more on this case and more education! @GrahamAbra @arvindcanchi @kidneydoc101 @caioqualunque
@goKDIGO @KatieKwonMD @kdjhaveri @ChristosArgyrop @logiebear111 @SLeonMD @nephondemand @ASNKidney @CardioNerds
@goKDIGO @KatieKwonMD @kdjhaveri @ChristosArgyrop @logiebear111 @SLeonMD @nephondemand @ASNKidney @CardioNerds
11) Welcome back! There's more to go on managing #hyperkalemia with the latest, safest options. I'm @edgarvlermamd. Encourage your colleagues, fellows, and residents to follow us here at @cardiomet_CE for serialized Twitter-based accredited education!
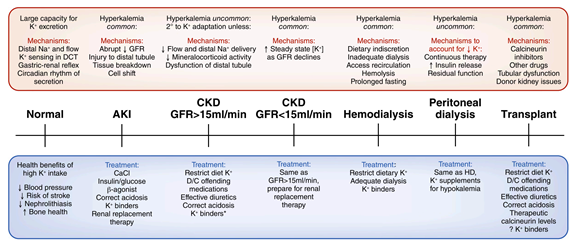
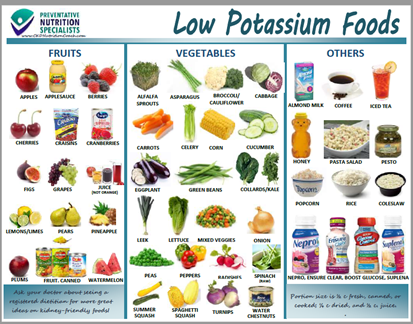
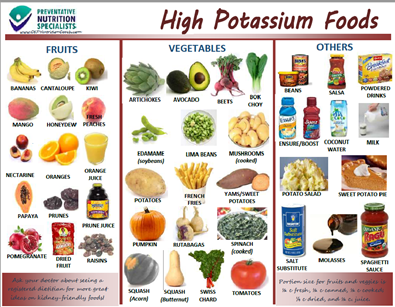
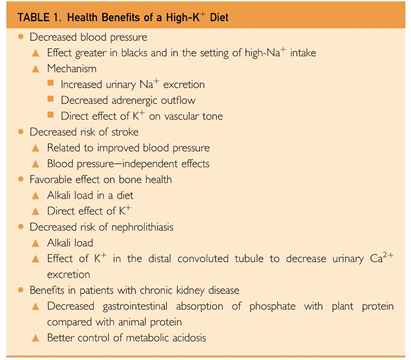
13) A low-K+ diet is difficult for patients to adhere to, particularly those who may have additional dietary restrictions due to #diabetes and reduced sodium intake for CKD or #heartfailure.
16) Despite beneficial effects of diuretics on volume status and BP, they may increase the risk of gout, volume depletion, decreased distal tubule flow, worsening kidney function, & reduced K+ excretion. Their effectiveness in managing hyperK+ relies on residual kidney function.
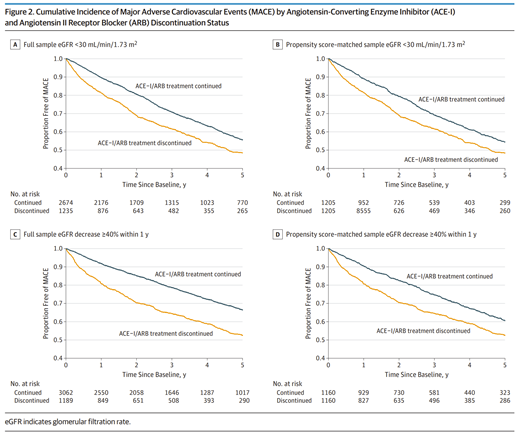
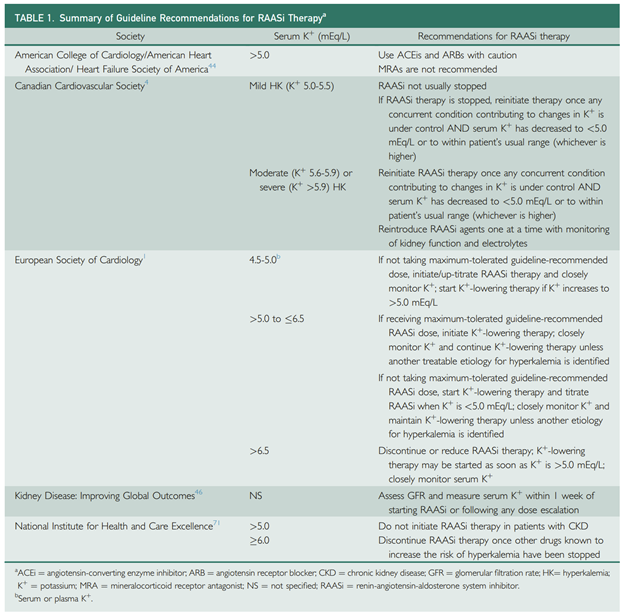
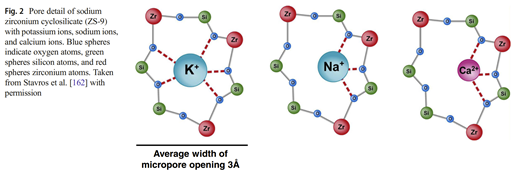
18) Discontinuation or dose reduction of #RAASi therapy may lead to adverse cardiorenal outcomes, and current guidelines differ with regard to recommendations on when to reinitiate RAASi.
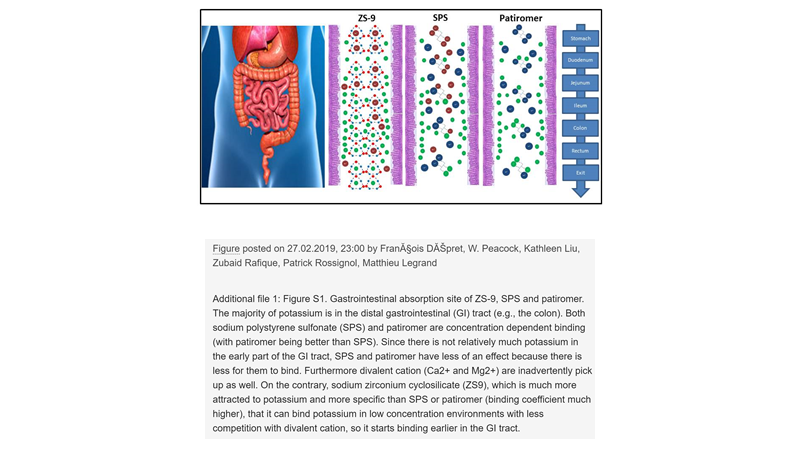
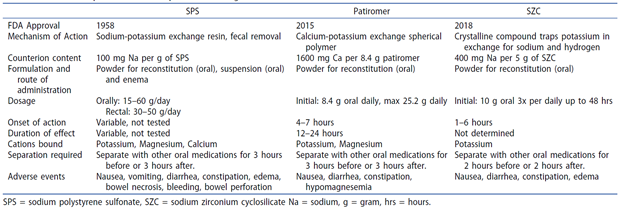
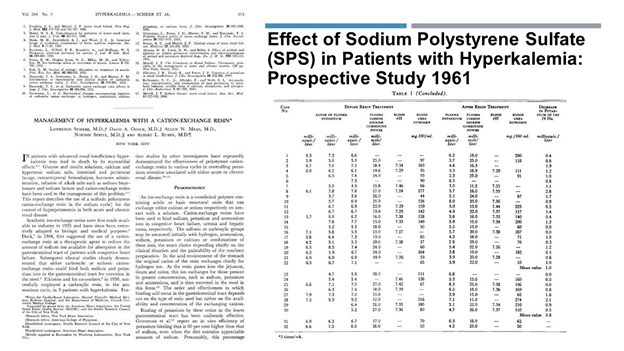
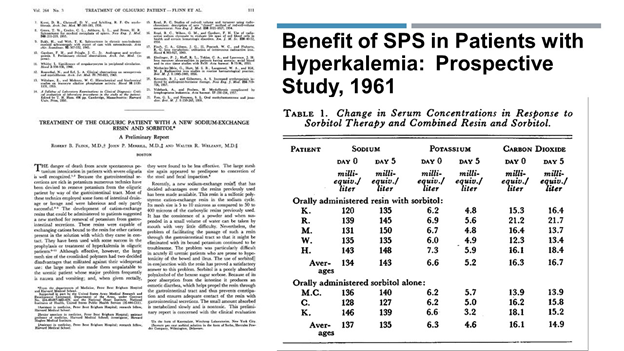
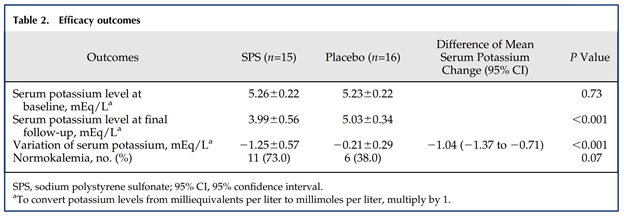
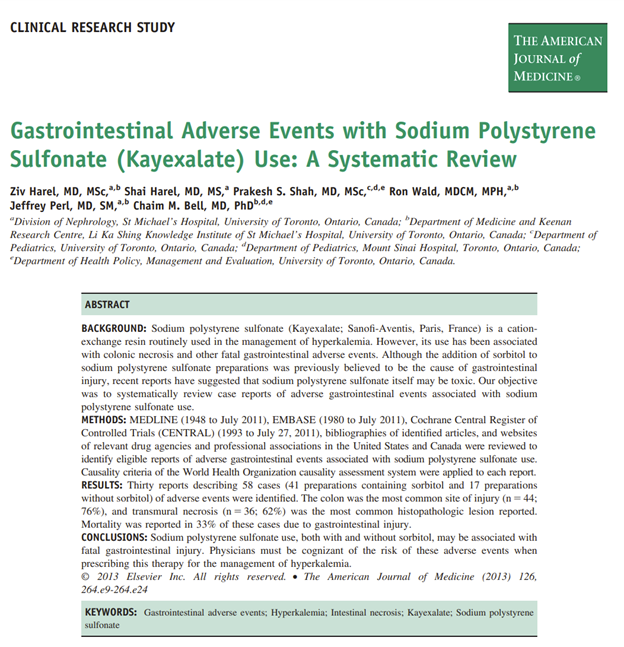
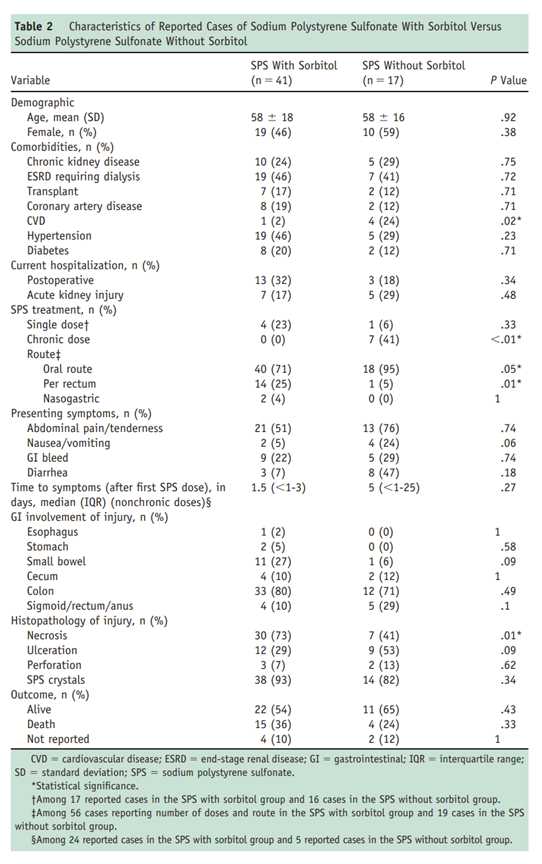
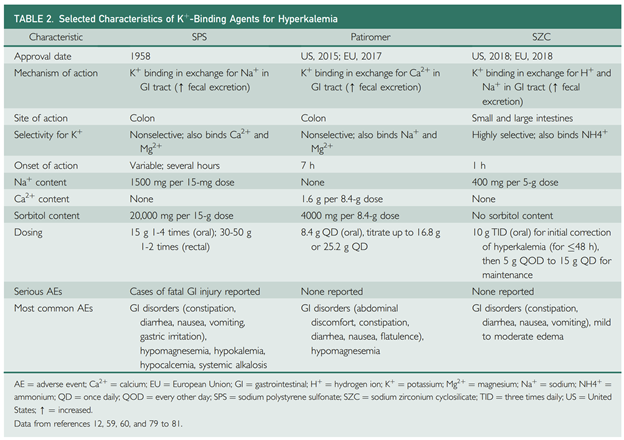
22) SPS is a polymeric cation-exchange resin that binds K+ ions in exchange for Na+ ions in the distal colon. It is nonselective for K+, with affinity for Ca2+ and Mg2+ ions. It may be given either orally or rectally (oral has poor palatability).
25) Do you know these drugs? What is/are the counter-ion for K+ exchange with SZC?
26) Mark your answer and return tomorrow for a detailed exploration of these new binders and a link to your free CE/#CME! @dr_nikhilshah @RenalFellowNtwk @HecmagsMD @Nephro_Sparks @AnnaGaddy @PharmERToxGuy @AliMehdiMD @ISNkidneycare @beaverspharmd @JamesNovakNeph
27) Welcome back! You are just a few clicks away from free #CME/CE. We are talking #hyperkalemia! I am @edgarvlermamd and this program is accredited by @academiccme. Previous programs (and credit!) available at cardiometabolic-ce.com.
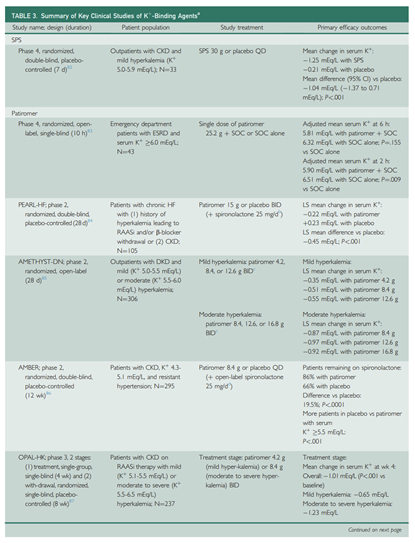
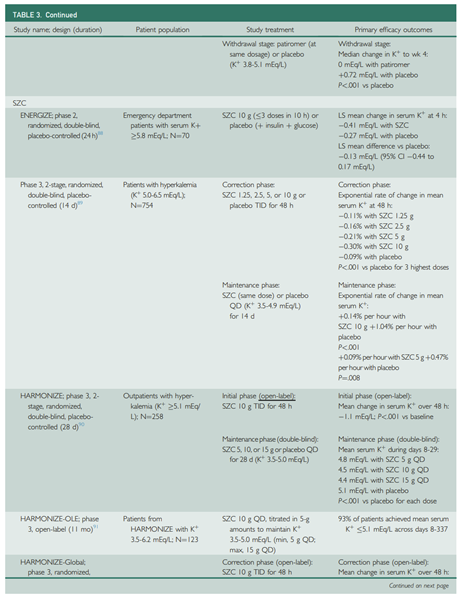
28) Oral patiromer contains a Ca2+ sorbitol counterion that exchanges Ca2+ for K+ as it passes through the colon. Like SPS, it is a polymer that is nonselective for K+ and may also bind Mg2+ and small amounts of Na+.
29) Patiromer’s time to onset of action is approximately 7 hours. Administration should be separated from other oral medications by ≥ 3 hours because of the potential for binding.
30) Unlike SPS and patiromer, SZC is nonpolymeric with high selectivity for K+ and NH4+ ions (1.25-fold higher affinity for K+ vs NH4+) in exchange for H+ and Na+ throughout the GIT. SZC binds monovalent cations (K+) as opposed to divalent cations (e.g., Ca2+ and Mg2+).
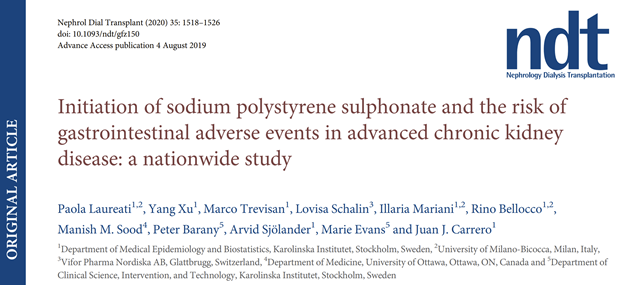
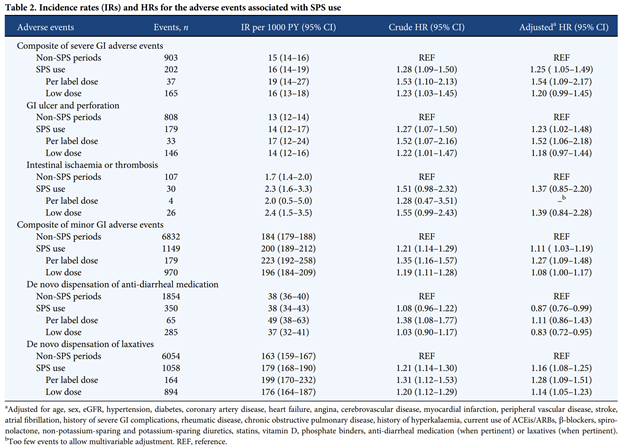
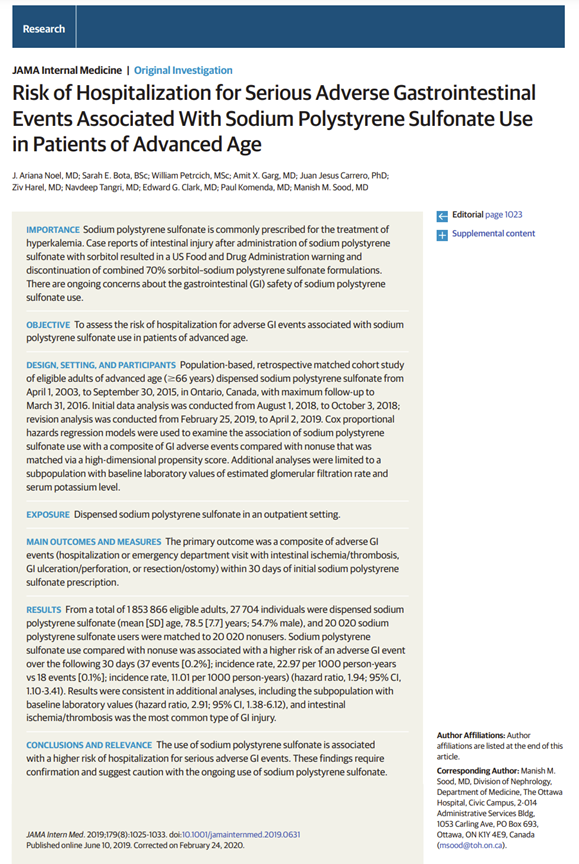
35) Although cohort studies have reported a higher relative risk of gastrointestinal AEs, the incidence of events with SPS was rare (16 or 23 events per 1000 person-years).
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
36) The most common AEs associated with patiromer therapy include gastrointestinal events (constipation, diarrhea, nausea/ vomiting, abdominal discomfort, and flatulence) and electrolyte disturbances (hypokalemia and hypomagnesemia) . . . as per
37) Like Patiromer, Sodium zirconium cyclosilicate has not been associated with any serious AEs in randomized trials. The most common AEs were hypokalemia and a dose-dependent increase in edema
nejm.org
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
nejm.org
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
38) The initiation of newer K+-binding agents should be considered in patients with chronic hyperkalemia despite optimized diuretic therapy and correction of metabolic acidosis.
39) After starting therapy at the recommended dose, K+ binders should be titrated for optimization of serum K+ concentration, with individualized monitoring of serum or plasma K+. Long-term K+-binder tx may be considered in patients with chronic hyperK as in the case presented.
40) The use of one of the newer K+-binding agents (SZC or patiromer) may allow for the continuation and optimization of #RAASi therapy in patients with #hyperkalemia.
42) That's it! You made it! Free CE/#CME! Now, all you #physicians, #nurses, and #pharmacists, go to cardiometabolic-ce.com and claim your credit from @academiccme! I am @edgarvlermamd. Follow @cardiomet_CE for more tweetorials! #medtwittter #nephtwitter @MedTweetorials #FOAMed
Loading suggestions...