A #tweetorial on non-variceal upper gastrointestinal bleeding #NVUGIB
And an overview of why we do what we do
To warm up, which of the following is the most common cause of NVUGIB?
#gitwitter #livertwitter #medtwitter #MedEd
1/
And an overview of why we do what we do
To warm up, which of the following is the most common cause of NVUGIB?
#gitwitter #livertwitter #medtwitter #MedEd
1/
5/
Syncope or fainting, is such a bad presenting symptom it's included in one of the risk stratification scores known as the Glasgow-Blatchford score (GBS)
Scoring 0⃣ means a low risk of complications and these patients may not need to be admitted
thelancet.com
Syncope or fainting, is such a bad presenting symptom it's included in one of the risk stratification scores known as the Glasgow-Blatchford score (GBS)
Scoring 0⃣ means a low risk of complications and these patients may not need to be admitted
thelancet.com
6/
A thorough history taking and physical examination is essential:
🧠 mental status
🚫 acute abdomen (ie shouldn't scope and need imaging/surgeon input)
💊 antiplatelets, anticoagulant use
A thorough history taking and physical examination is essential:
🧠 mental status
🚫 acute abdomen (ie shouldn't scope and need imaging/surgeon input)
💊 antiplatelets, anticoagulant use
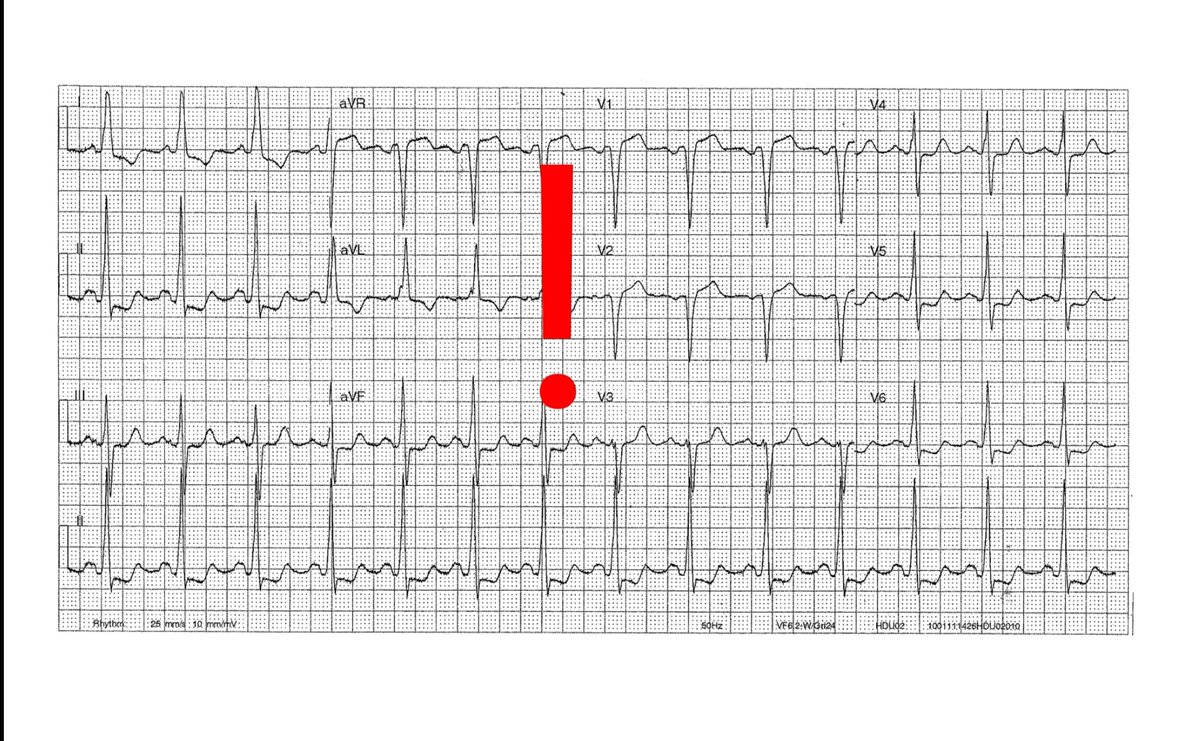
8/
Besides blood taking, 🔬 Ix we routinely request include:
- erect CXR (any free gas, weird funny mediastinal gas)
- ECG (acute coronary syndrome)
&
- #covid19 in this day and age
Besides blood taking, 🔬 Ix we routinely request include:
- erect CXR (any free gas, weird funny mediastinal gas)
- ECG (acute coronary syndrome)
&
- #covid19 in this day and age
9/
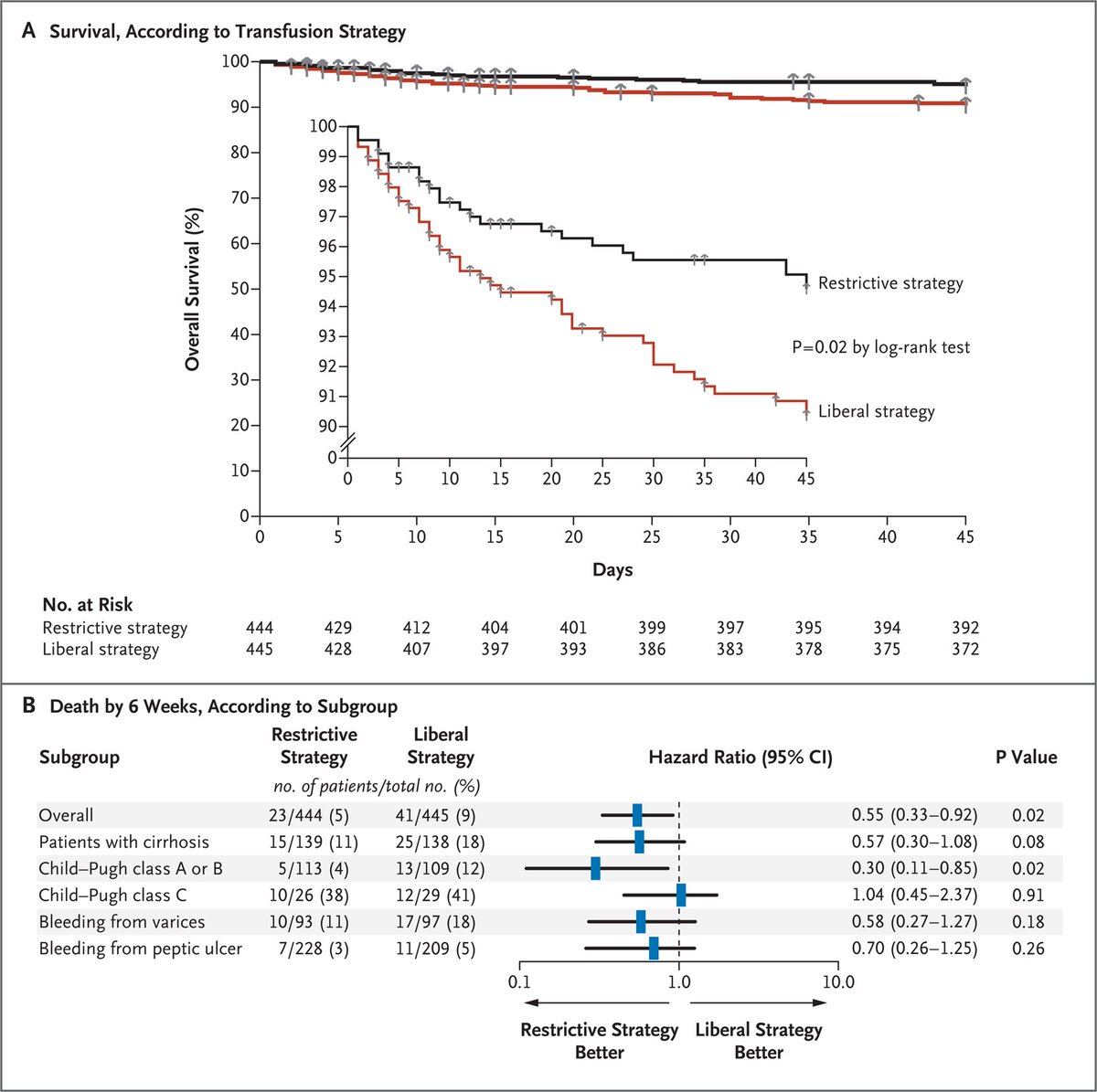
Restrictive transfusion with a Hb >= 7 g/dL is likely sufficient for most hemodynamically stable patients
Subgroup showed that this was better for Child's A/B (postulated that ⬆️splanchnic pressure ➡️ rebleeding, fluid overload, other transfusion Cx)
nejm.org
Restrictive transfusion with a Hb >= 7 g/dL is likely sufficient for most hemodynamically stable patients
Subgroup showed that this was better for Child's A/B (postulated that ⬆️splanchnic pressure ➡️ rebleeding, fluid overload, other transfusion Cx)
nejm.org
12/
❌ Drugs to stop i.e. DAPTs, anticoagulants
Always ⚖️ risks (of thromboembolism) and benefits (easier hemostasis)
Risks of PUD re-bleeding ⬆️ in first 3⃣ days
The 2021 @ESGE_news guidelines in @endoscopyjrnl shared by @drkeithsiau are great!
❌ Drugs to stop i.e. DAPTs, anticoagulants
Always ⚖️ risks (of thromboembolism) and benefits (easier hemostasis)
Risks of PUD re-bleeding ⬆️ in first 3⃣ days
The 2021 @ESGE_news guidelines in @endoscopyjrnl shared by @drkeithsiau are great!
14/
And for a thread discussing the GI safety and efficacy of #DOACs here's the link 👇
In summary: seems that apixaban has a more favourable GI safety profile (no COI)
And for a thread discussing the GI safety and efficacy of #DOACs here's the link 👇
In summary: seems that apixaban has a more favourable GI safety profile (no COI)
15/
In hemodynamically unstable cases or uncontrolled bleeding reversal agents may also need to be considered
In hemodynamically unstable cases or uncontrolled bleeding reversal agents may also need to be considered
16/
Finally we arrive at peri-endoscopic mx!
Wt is the role of pre-endoscopy prokinetics?
- A MA in @GIE_Journal showed that erythromycin or metoclopromide given immediately before OGD/EGD ⬇️ the need for repeat endoscopy but not other parameters
ncbi.nlm.nih.gov
Finally we arrive at peri-endoscopic mx!
Wt is the role of pre-endoscopy prokinetics?
- A MA in @GIE_Journal showed that erythromycin or metoclopromide given immediately before OGD/EGD ⬇️ the need for repeat endoscopy but not other parameters
ncbi.nlm.nih.gov
17/
How about PPIs?
A landmark trial by Prof Lau @CUHKMedicine showed that pre-emptive PPI infusion:
⬇️ Endoscopic grade of lesions
⬇️ Need for endoscopic treatment
↔️ Similar rates of recurrent bleeding, surgery and 30-day ☠
nejm.org
How about PPIs?
A landmark trial by Prof Lau @CUHKMedicine showed that pre-emptive PPI infusion:
⬇️ Endoscopic grade of lesions
⬇️ Need for endoscopic treatment
↔️ Similar rates of recurrent bleeding, surgery and 30-day ☠
nejm.org
20/
So we finally arrive to the point where we put a scope in
We classify the endoscopic appearance of ulcers by the Forrest classification with great examples by @EndoscopyCampus endoscopy-campus.com
The rebleeding rates (w/o therapy) are tabulated here
So we finally arrive to the point where we put a scope in
We classify the endoscopic appearance of ulcers by the Forrest classification with great examples by @EndoscopyCampus endoscopy-campus.com
The rebleeding rates (w/o therapy) are tabulated here
22/
So what's the role of PPI after endoscopy?
2 RCTs again led by my mentors @CUHKMedicine showed that 72h of PPIs afterwards
⬇️Rebleeding
⬇️Need of Surgery
But didnt show a sig difference for reducing mortality
So what's the role of PPI after endoscopy?
2 RCTs again led by my mentors @CUHKMedicine showed that 72h of PPIs afterwards
⬇️Rebleeding
⬇️Need of Surgery
But didnt show a sig difference for reducing mortality
24/
Excellent reading materials for further interest
@BritSocGastro #AUGIB care bundle
fg.bmj.com
A great updated review in DEN
onlinelibrary.wiley.com
Excellent reading materials for further interest
@BritSocGastro #AUGIB care bundle
fg.bmj.com
A great updated review in DEN
onlinelibrary.wiley.com
25/
To conclude:
- risk stratification
- Mx: ABC and DAVIDS
- restrictive transfusion unless hemodynamically unstable, ischemic events
- ❌endoscopy if perforation, IO
- tx pre, during and post endoscopy
- balance risk and benefits on resumption of antiplatelets/anticoagulants
To conclude:
- risk stratification
- Mx: ABC and DAVIDS
- restrictive transfusion unless hemodynamically unstable, ischemic events
- ❌endoscopy if perforation, IO
- tx pre, during and post endoscopy
- balance risk and benefits on resumption of antiplatelets/anticoagulants
Loading suggestions...