Some quick hits on 🗣️ PE as a cause of pleural effusions 🗣️ – listen up, because this is the 4th leading cause of effusions in the U.S.! 👍 karger.com
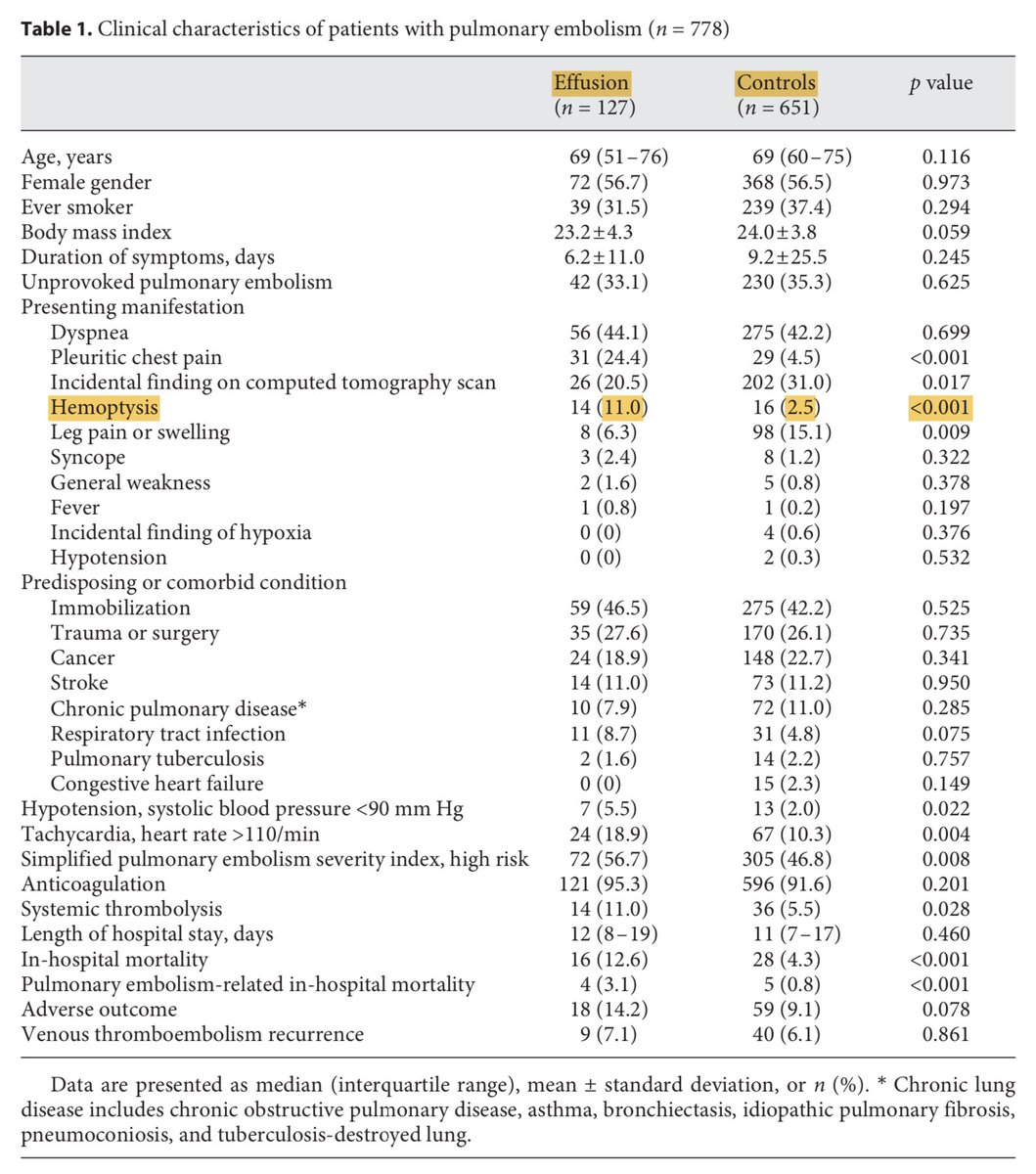
This is such a simple, elegant study. 127 patients w/ CT-diagnosed PE + effusion, and 651 CT-diagnosed PEs without effusion. The authors excluded patients with major comorbid causes of effusion (eg malignancy).
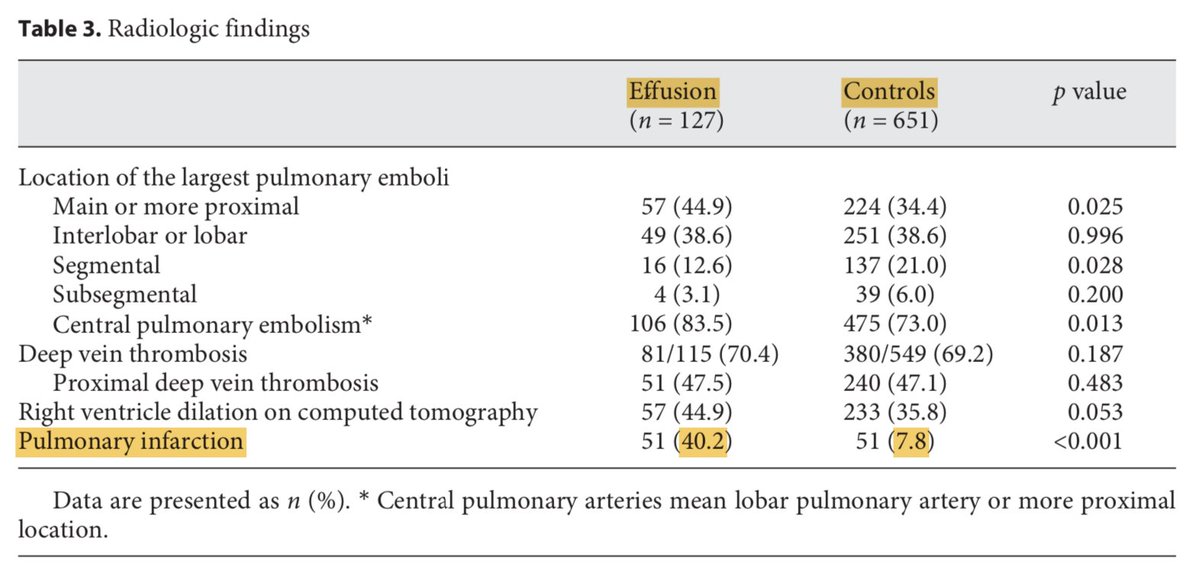
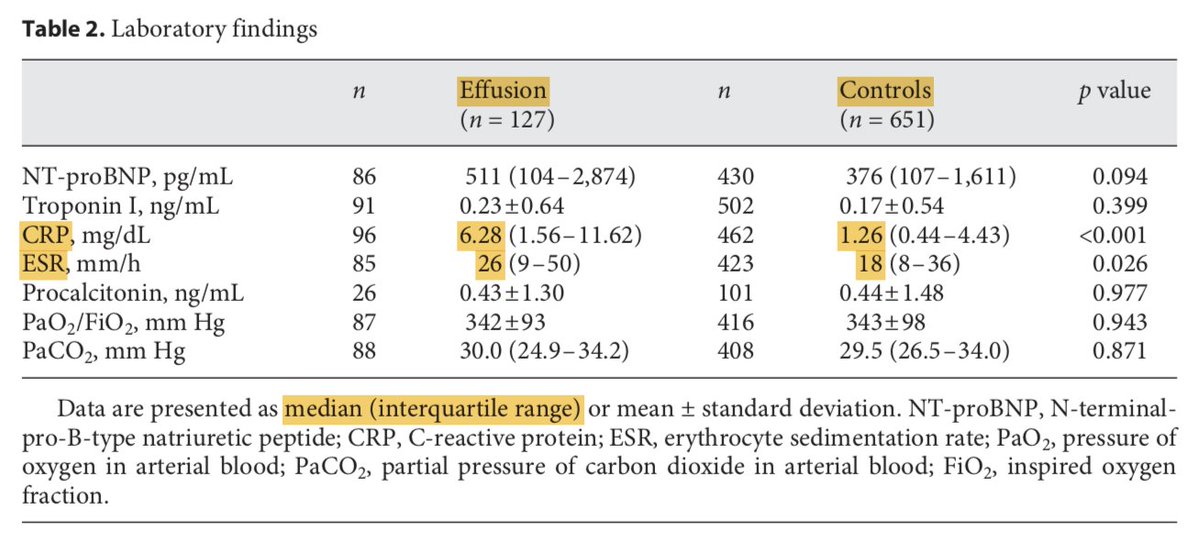
2) On multivariate analysis, pulmonary infarction (OR 6.20, 95% CI 3.49-10.91) & CRP levels (OR 1.05, 95% CI 1.101-1.09) were independent predictors of effusions due to PE. Infarction defined as the presence of a peripheral consolidation in the region of a (sub)segmental PE.
4) Most (92%) effusions that got tapped were exudative. Proposed mechanism: platelet-rich emboli ➡️ inflammatory mediator release ➡️ leaky pulm capillaries ➡️ interstit. fluid passes through visceral pleura ➡️ effusion! This is interesting because...
And that's it for fun #pulm facts today! Thanks for reading 👍
Loading suggestions...