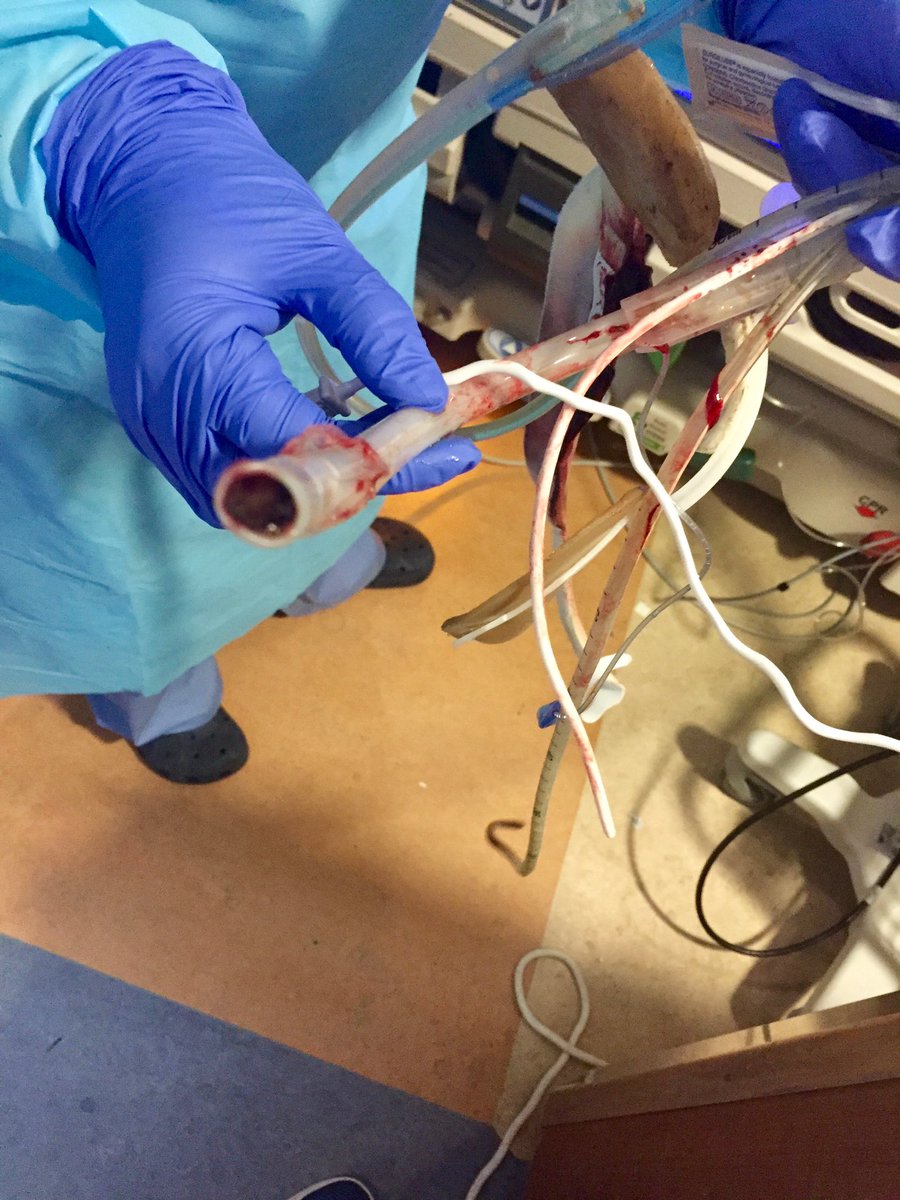
Interesting issue in mechanical ventilation of #COVID19 patients, each one here after >10 days of mechanical ventilation.
How might we monitor for development of this? Time to pay attention to resistance, oft neglected in the age of COVID #ARDS...
#tweetorial #SoMe4MV
How might we monitor for development of this? Time to pay attention to resistance, oft neglected in the age of COVID #ARDS...
#tweetorial #SoMe4MV
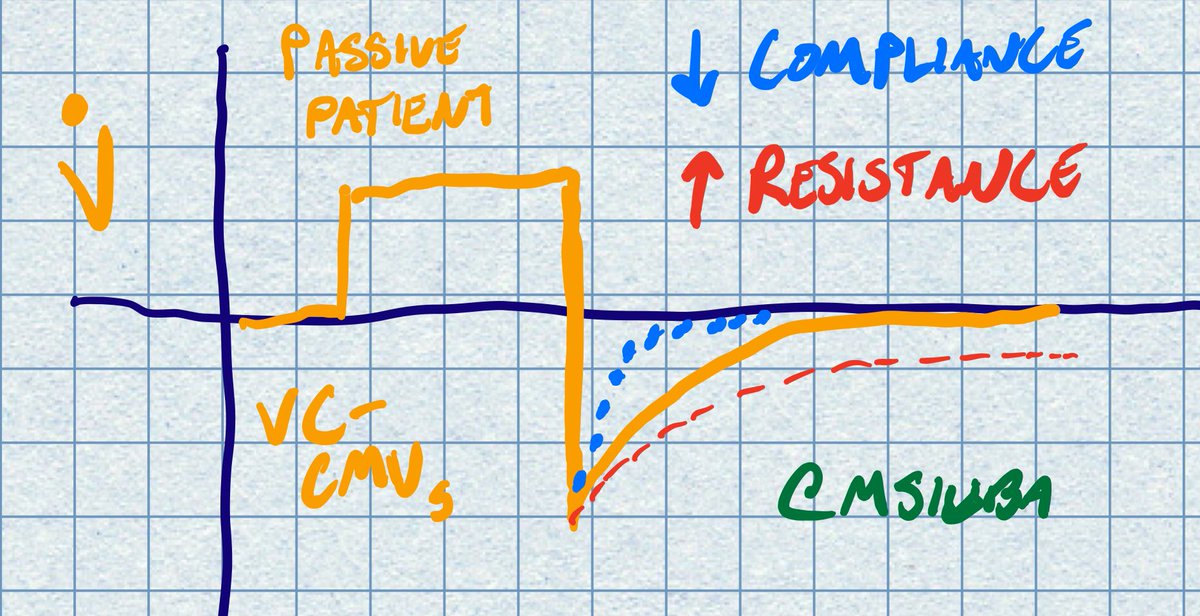
First step is to examine the flow waveform. In this case a patient in volume control, to observe how passive expiration is changed by changing time constant.
More on time constants here: derangedphysiology.com
More on time constants here: derangedphysiology.com
A faster time constant is associated with decreased compliance (increased elastic recoil). The opposite is seen with airway resistance.
In these cases we often see the expiratory phase on the flow diagram *not* return to baseline before the next inspiration is initiated
In these cases we often see the expiratory phase on the flow diagram *not* return to baseline before the next inspiration is initiated
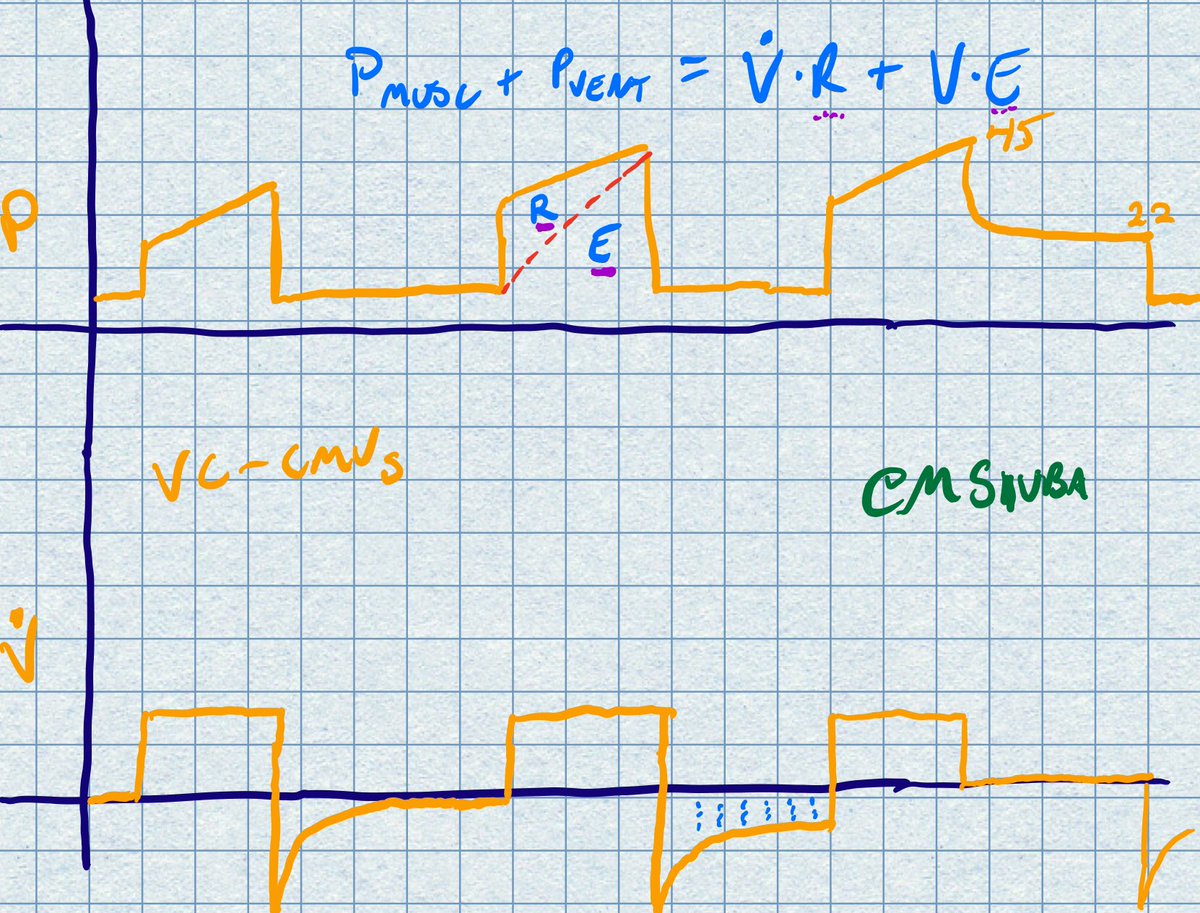
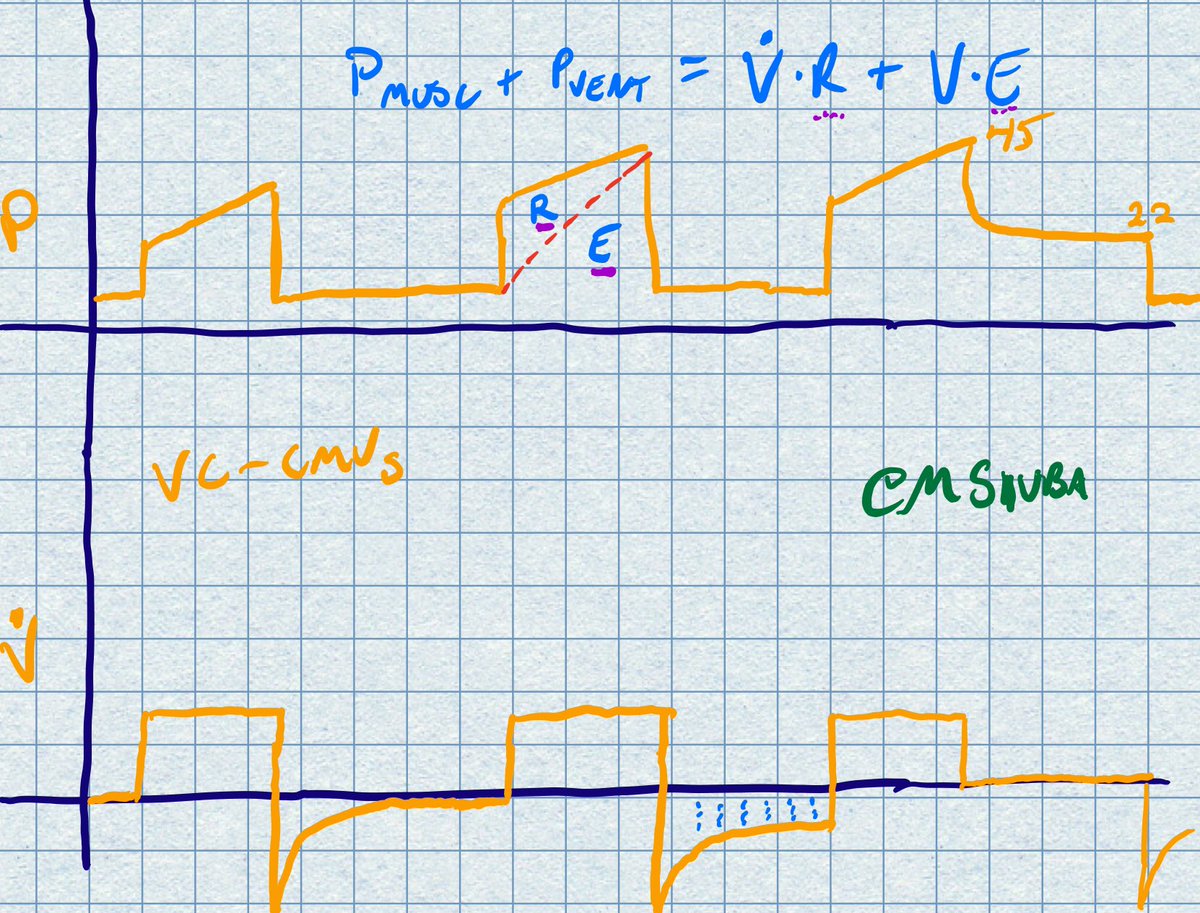
That last breath shows a plateau pause. This helps to diagnose the cause of elevated Ppeak. Looking at the equation of motion, a plateau pause would eliminate the contribution of resistance to the pressure (because flow = 0).
Larger delta between Ppeak and Pplat suggests ⬆️R
Larger delta between Ppeak and Pplat suggests ⬆️R
In sum,
⬆️R can be dx by:
- ⬆️ time constant
- Failure of flow to return to baseline
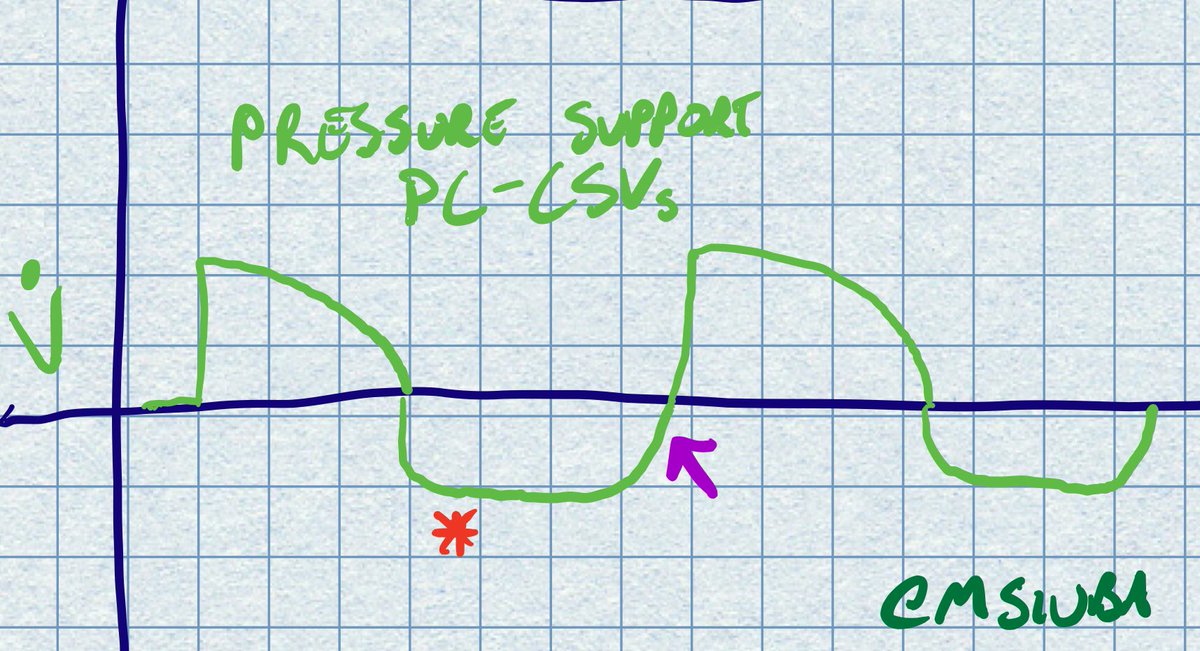
- Forceful exhale
- ⬆️Ppeak with large delta of Peak - Plat
? on this in #COVID19 patients, especially after a few days on the vent
Don’t forget typical causes of ⬆️R, including asthma/COPD
⬆️R can be dx by:
- ⬆️ time constant
- Failure of flow to return to baseline
- Forceful exhale
- ⬆️Ppeak with large delta of Peak - Plat
? on this in #COVID19 patients, especially after a few days on the vent
Don’t forget typical causes of ⬆️R, including asthma/COPD
Loading suggestions...