1/21 After caring for patients in the ICU with #COVID for the last week, the time seems right for a #pulmonology #tweetorial on #Proning or #PronePositioning
@sanjayvdesai @OslerResidency @JHUPCCMFellows @CPSolvers @thecurbsiders @cardionerds @tony_breu @david_furfaro @chadhoc
@sanjayvdesai @OslerResidency @JHUPCCMFellows @CPSolvers @thecurbsiders @cardionerds @tony_breu @david_furfaro @chadhoc
2/ Let’s begin with a question: how does prone positioning improve oxygenation in patients with severe Acute Respiratory Distress Syndrome (ARDS)?
3/ First, some history. Prone positioning was first proposed in the 1970’s as a method to improve gas exchange in resp. failure and has long been shown to improve Pa/FiO2 in mechanically ventilated patients with severe ARDS.
ncbi.nlm.nih.gov
ncbi.nlm.nih.gov
ncbi.nlm.nih.gov
ncbi.nlm.nih.gov
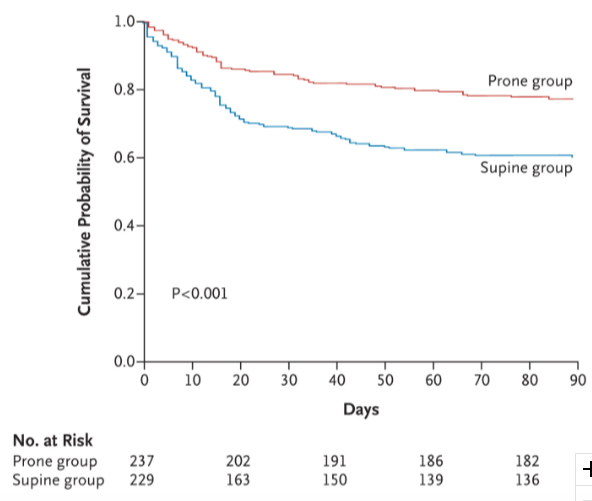
4/ However, translating physiologic improvements into clinical benefit proved challenging. It wasn’t until the NEJM PROSEVA trial that prone positioning became widely accepted as an effective therapy to reduce mortality in severe ARDS. ncbi.nlm.nih.gov
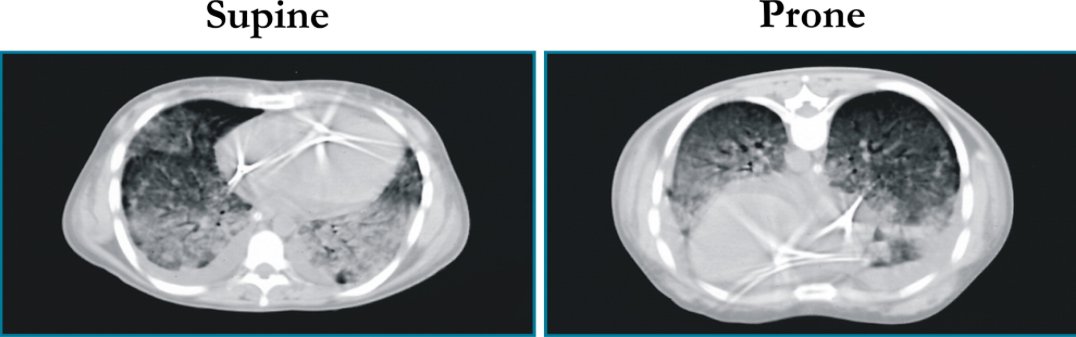
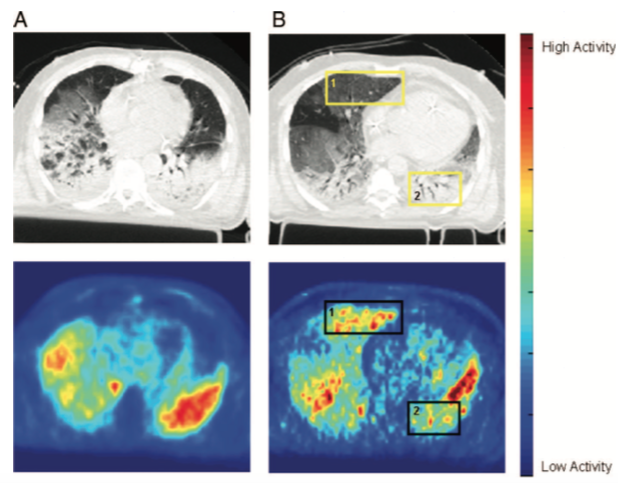
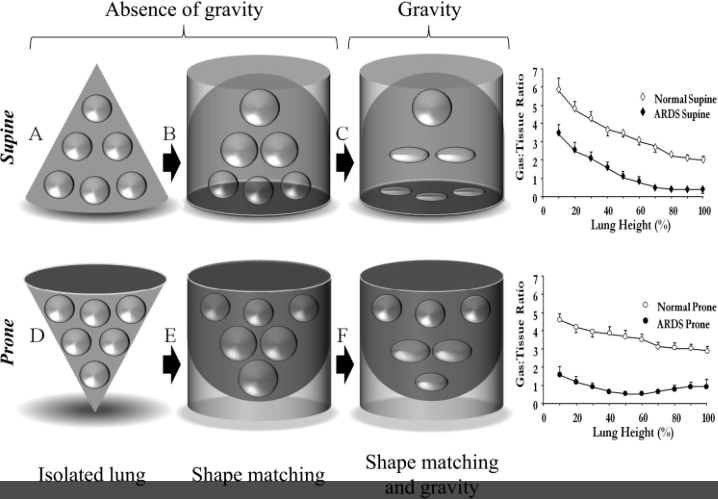
6/ First, let’s look at redistribution of blood flow. Studies in animals and humans (using PET) have shown that blood flow distribution in the lung does not change substantially from supine to prone position in ARDS.
ncbi.nlm.nih.gov
ncbi.nlm.nih.gov
ncbi.nlm.nih.gov
ncbi.nlm.nih.gov
7/ How about increased chest wall compliance? The dorsal chest wall is actually LESS compliant than the ventral chest wall, which leads to an overall net decrease in chest wall compliance when prone since the ventral wall is impeded from expanding.
ncbi.nlm.nih.gov
ncbi.nlm.nih.gov
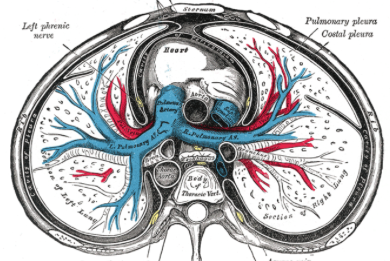
10/ When prone, the forces of gravity and “shape matching” oppose each other, which leads to more homogenous inflation of the pulmonary units from the sternum to vertebra.
11/ Additionally, the heart weight no longer compresses the left lower lobe and abdominal pressure is lessened.
12/ This leads to an overall recruitment in (larger) dorsal lung regions which outweighs the degree of derecruitment in the (smaller) ventral lung regions, leading to an overall increase in lung compliance.
ncbi.nlm.nih.gov
ncbi.nlm.nih.gov
13/ This also explains why we do not typically see an⬆️in Pplat (during VC vent.) or a⬇️in TV (during PC vent.) following pronation. Prone positioning also helps protect against Vent. Induced Lung Injury (VILI) by distributing stress and strain more homogeneously through the lung
14/ Here is a video courtesy of NEJM outlining the steps for prone positioning in mechanically ventilated patients (experienced staff is key!):
youtube.com
youtube.com
15/ So why is prone positioning so important in the #COVID pandemic? Based on clinical characteristic data from Wuhan, COVID often leads to ICU admission (15-20% of patients), ARDS (20% of patients), and mechanical ventilation (3% of patients).
ncbi.nlm.nih.gov
ncbi.nlm.nih.gov
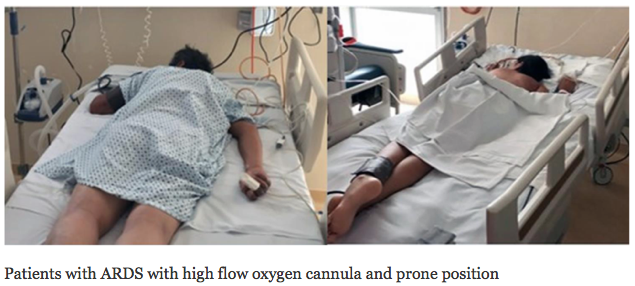
17/ Interestingly, small prospective cohort studies have showed that prone positioning combined with HFNC (or NIV) in patients with moderate ARDS (PaO2/FiO2 > 100) may help avoid intubation.
ncbi.nlm.nih.gov
ncbi.nlm.nih.gov
19/ With a looming shortage of vents, prone positioning with HFNC is a possible strategy to avoid intubation & its complications in patients with mod-to-severe ARDS, but more data is needed to assess safety & efficacy.
So let's revisit our original question: why does prone positioning improve oxygenation in patients with severe Acute Respiratory Distress Syndrome (ARDS)?
21/ SUMMARY:
✅ Prone positioning (PP) leads to more homogenous inflation of lungs
✅ This improves oxygenation, and reduces mortality in severe ARDS
✅ HFNC & PP is a possible strategy to consider to avoid intubation (especially in COVID pandemic), but more studies are needed
✅ Prone positioning (PP) leads to more homogenous inflation of lungs
✅ This improves oxygenation, and reduces mortality in severe ARDS
✅ HFNC & PP is a possible strategy to consider to avoid intubation (especially in COVID pandemic), but more studies are needed
Loading suggestions...