1/ In Dec. 2018, I posted my first #Tweetorial, on digestive tract neuroendocrine neoplasms. I polled Twitter asking what my next topic would be, and the winner was hepatic masses. More than a YEAR later, here it is! #pathology #liverpath
2/ Broad points: Most liver masses are benign, especially in younger patients. Older and cirrhotic patients are at increased risk for malignancy. Masses in cirrhosis are almost always primary liver malignancies (usually HCC).
5/ The new WHO 5th edition formally recognizes some variants, including diffuse hepatic hemangiomatosis, hepatic small vessel neoplasm, and anastomosing hemangioma (AH). Those last two may be the same thing? AH pic courtesy @cerubbsilva.
9/ Most cases of EHE have a WWTR1-CAMTA1 fusion, with corresponding nuclear CAMTA1 IHC positivity. Rare cases have YAP1-TFE3 instead and are positive for TFE3.
13/ A similar but super-rare lesion is biliary adenofibroma. (Never seen one -- pics from bit.ly) Large, solid/microcystic, can have malignant foci. Basically looks like a bigger, badder version of the past two entities.
15/ And now, cholangiocarcinoma, the “adenocarcinoma of the liver.” Most common in Southeast Asia. Risk factors include cirrhosis, liver fluke infection, and primary sclerosing cholangitis (but not primary biliary cirrhosis).
16/ It can form several gross patterns including mass-forming, periductal infiltrating, and intraductal. This used to matter for AJCC staging but no longer does!
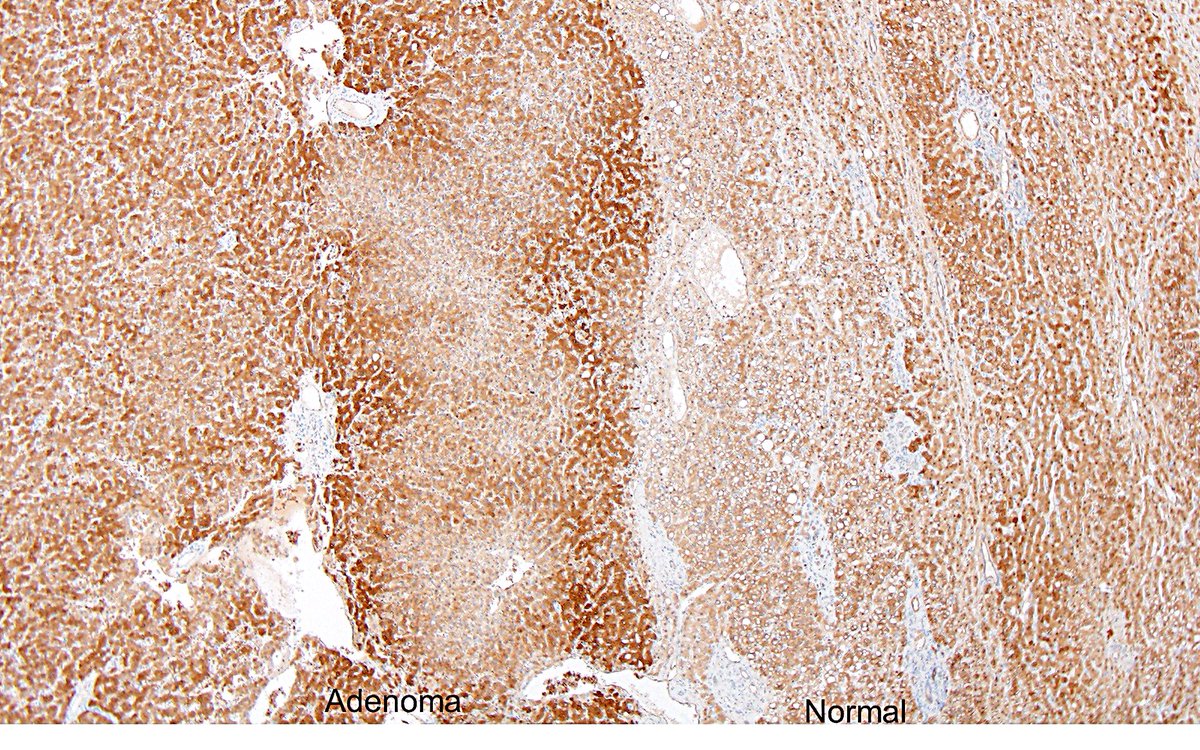
20/ The confusion (or fun) really begins with hepatocellular adenoma (HCA). Not that uncommon, usually arising in younger women on oral contraceptives. Can be large, can be multifocal, can rupture. Rarely turns malignant. So many subtypes!
25/ The final, vaguely defined HCA subtype is the sonic hedgehog variety. These are uncommon and tend to bleed. ASS1 IHC may help identify them (hey look, it’s the urea cycle!), but data are conflicting. Photo courtesy @rondell_graham.
27/ And on to hepatocellular carcinoma (HCC). Most common hepatic liver malignancy, 5th most common cancer worldwide. It typically arises in cirrhosis of any cause, though it can occur in non-cirrhotic livers (one cause: HBV).
32/ The most famous HCC subtype is also @rondell_graham’s favorite – fibrolamellar HCC! Has a central scar, just like FNH. Usually in younger, non-cirrhotic patients. Eosinophilic cells, prominent nuclei, fibrosis. DNAJB1-PRKACA fusion.
35/ Now to wander into combined HCC-cholangiocarcinoma. This concept and classification remain in flux. The current WHO does not define subtypes, instead simply requiring unequivocal hepatocytic and cholangiocytic differentiation on H&E.
37/ Finally, hepatoblastoma. (I’m not a peds pathologist and I never see these.) Most common liver tumor, mostly in children under age 5. Linked to many syndromes (FAP, Beckwith–Wiedemann, etc.). COG staging system, based on resectability.
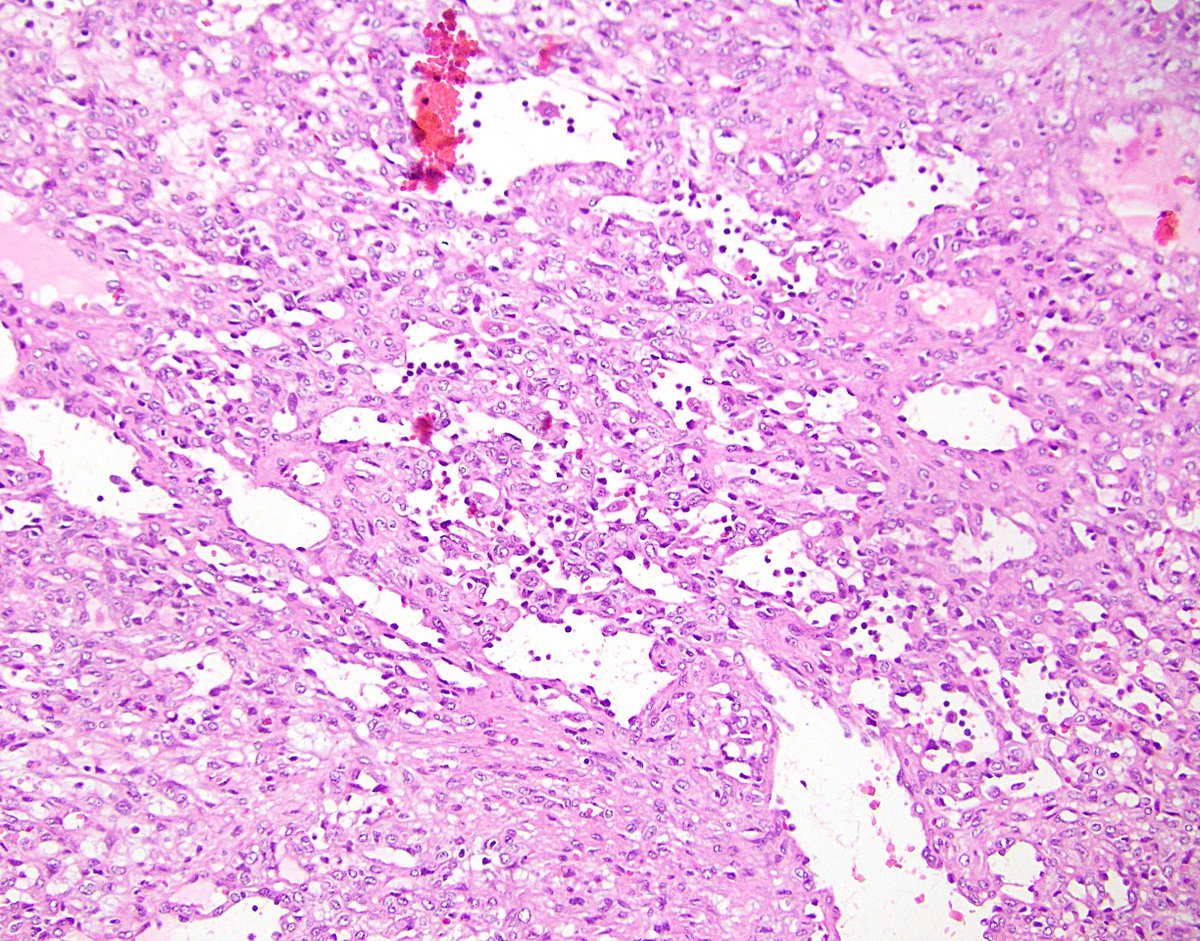
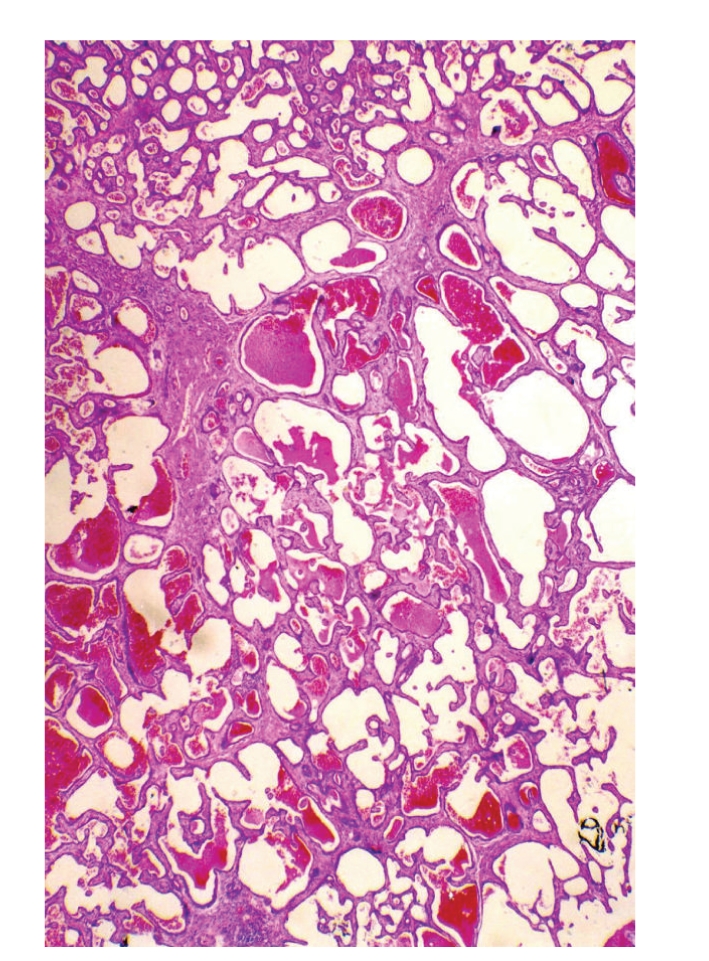
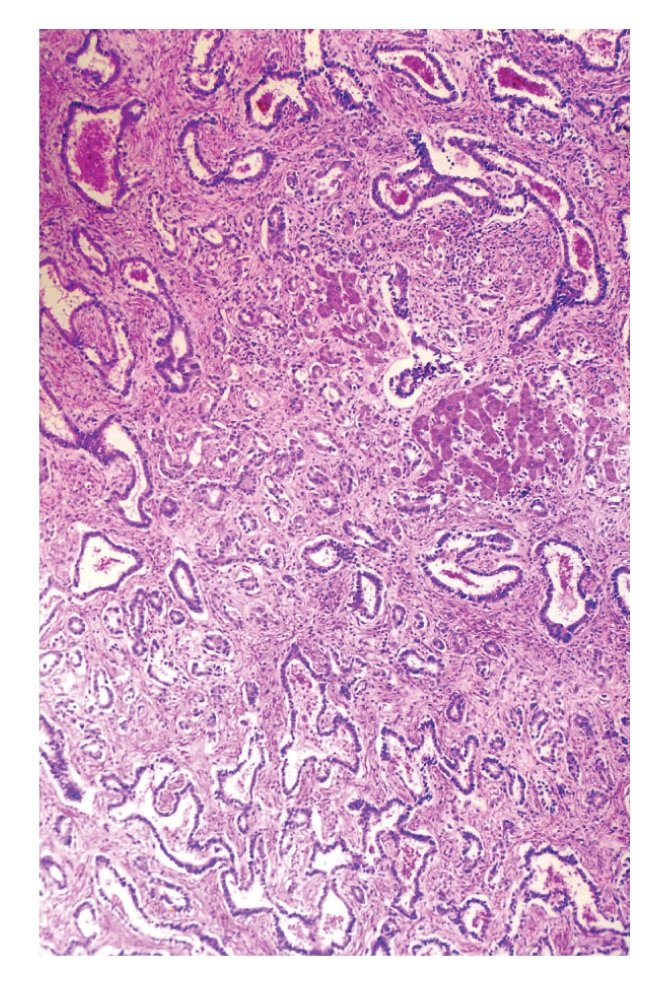
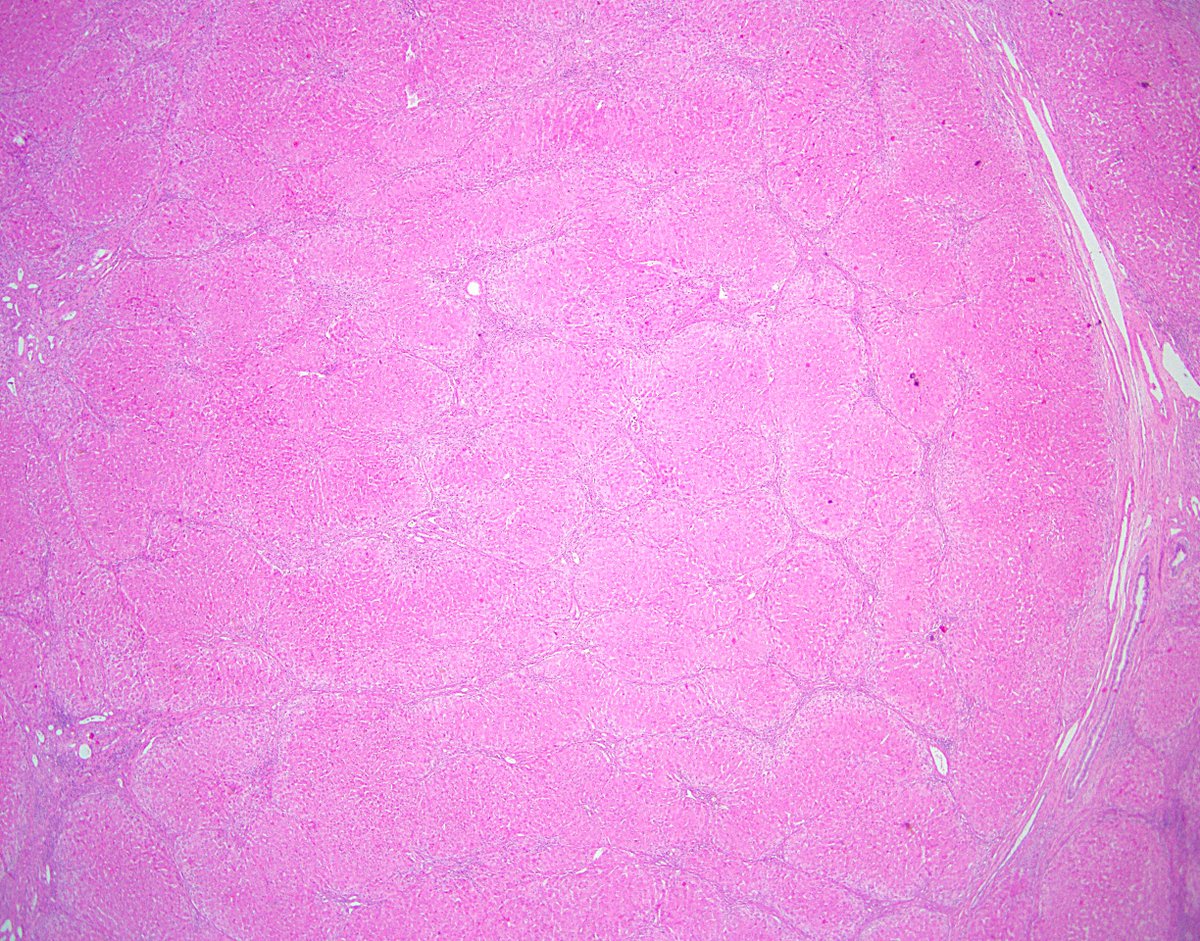
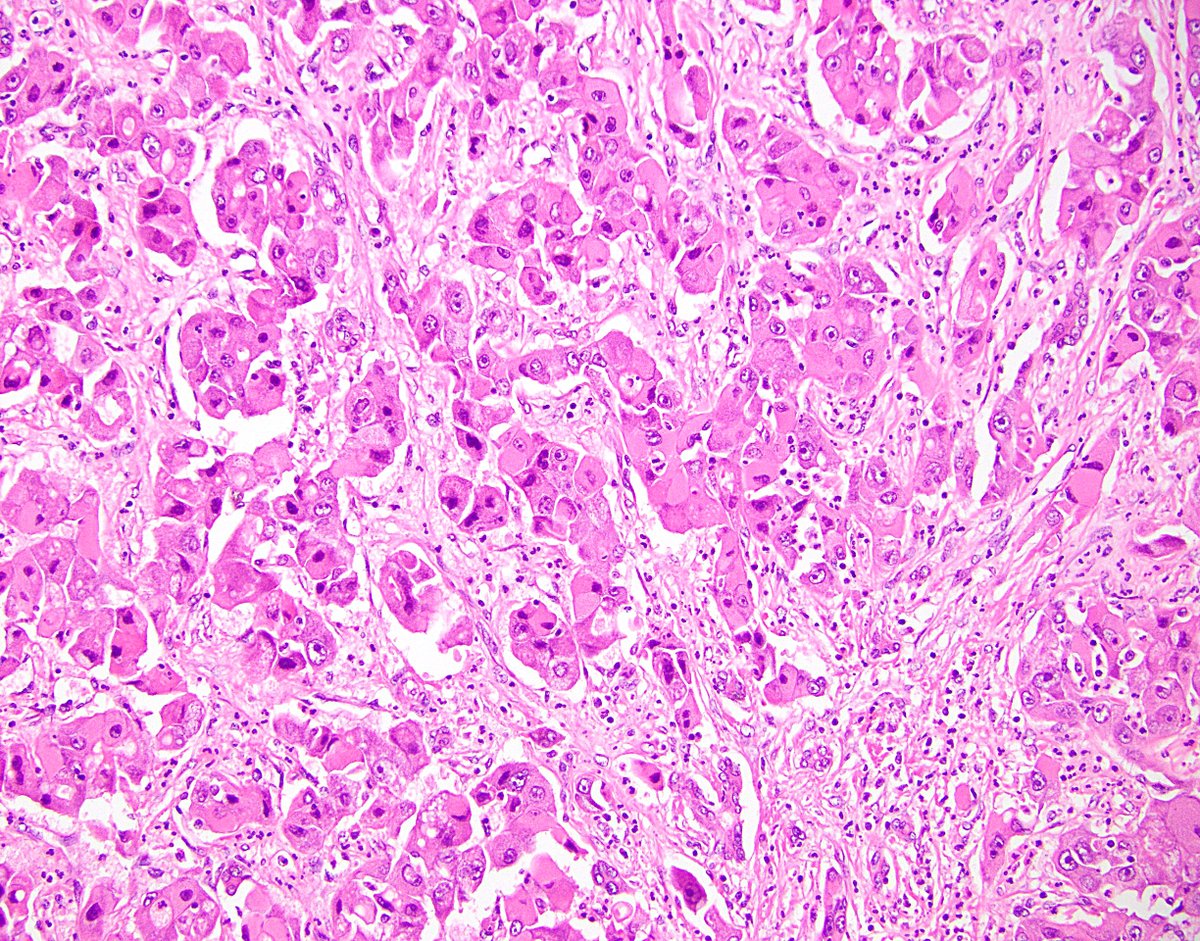
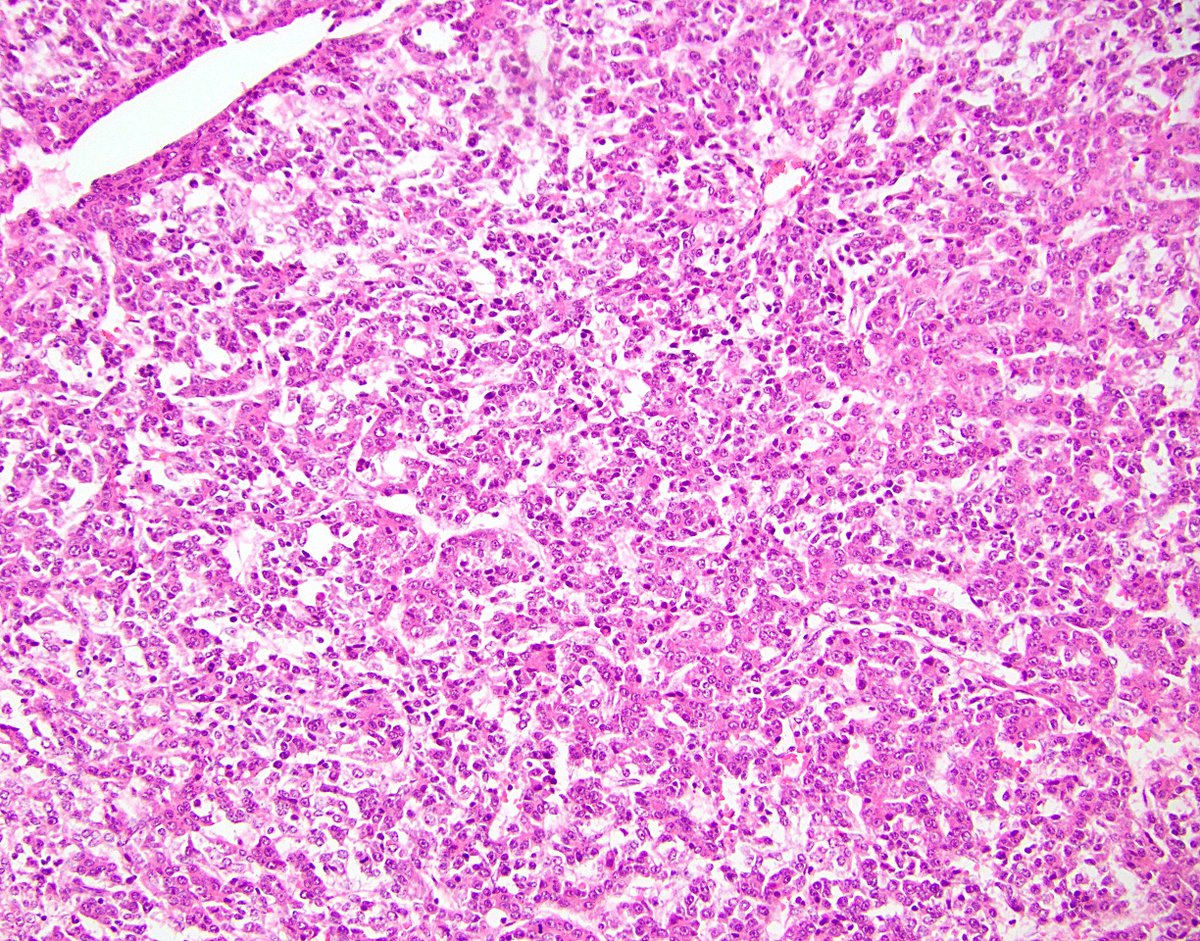
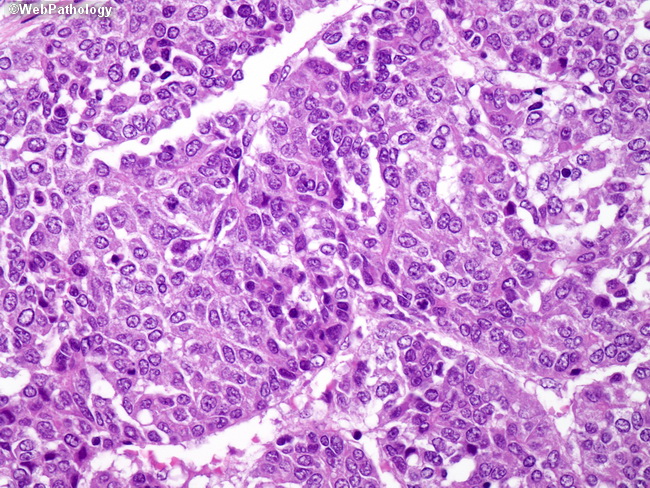
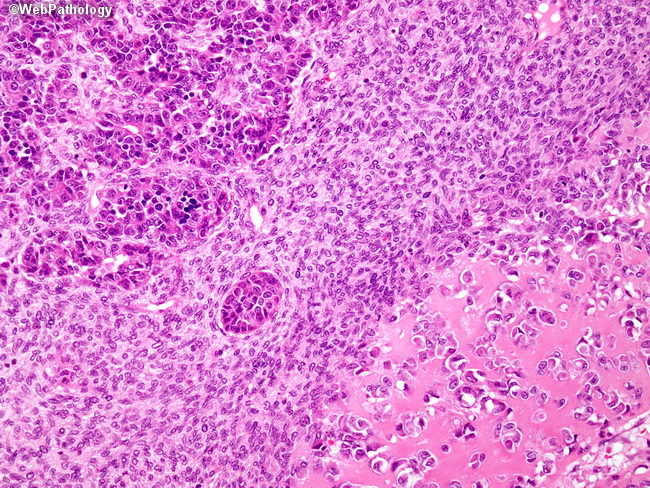
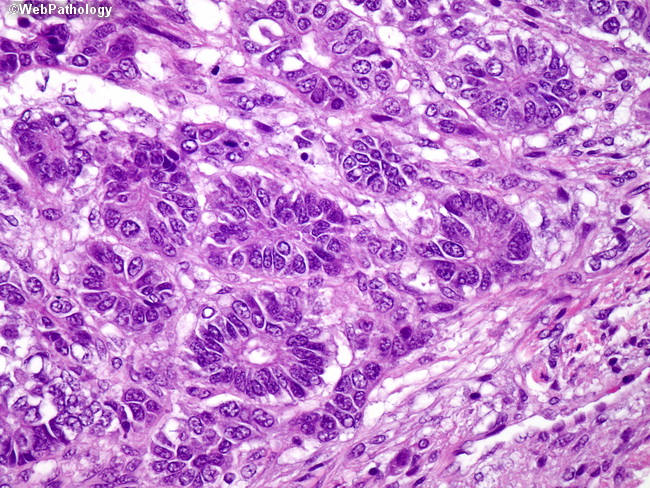
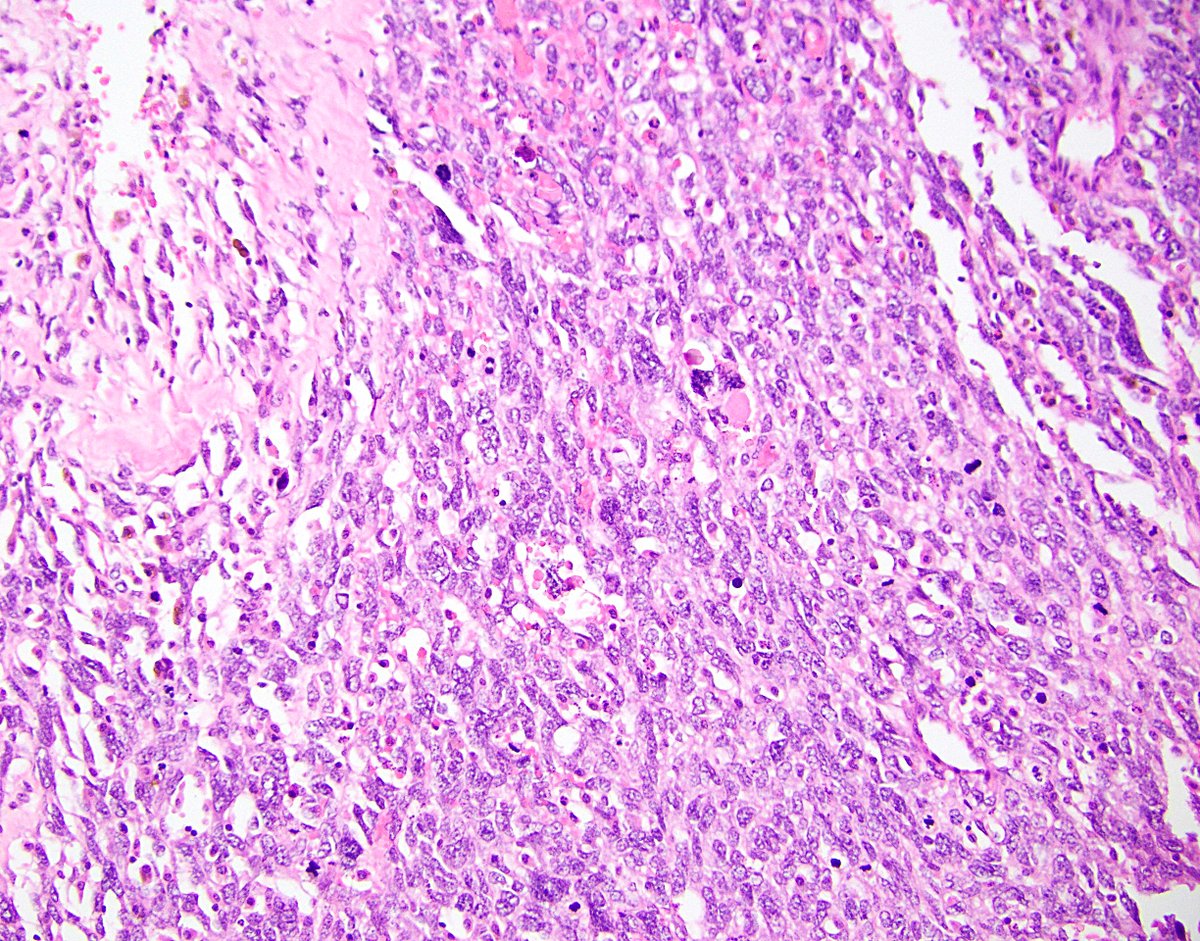
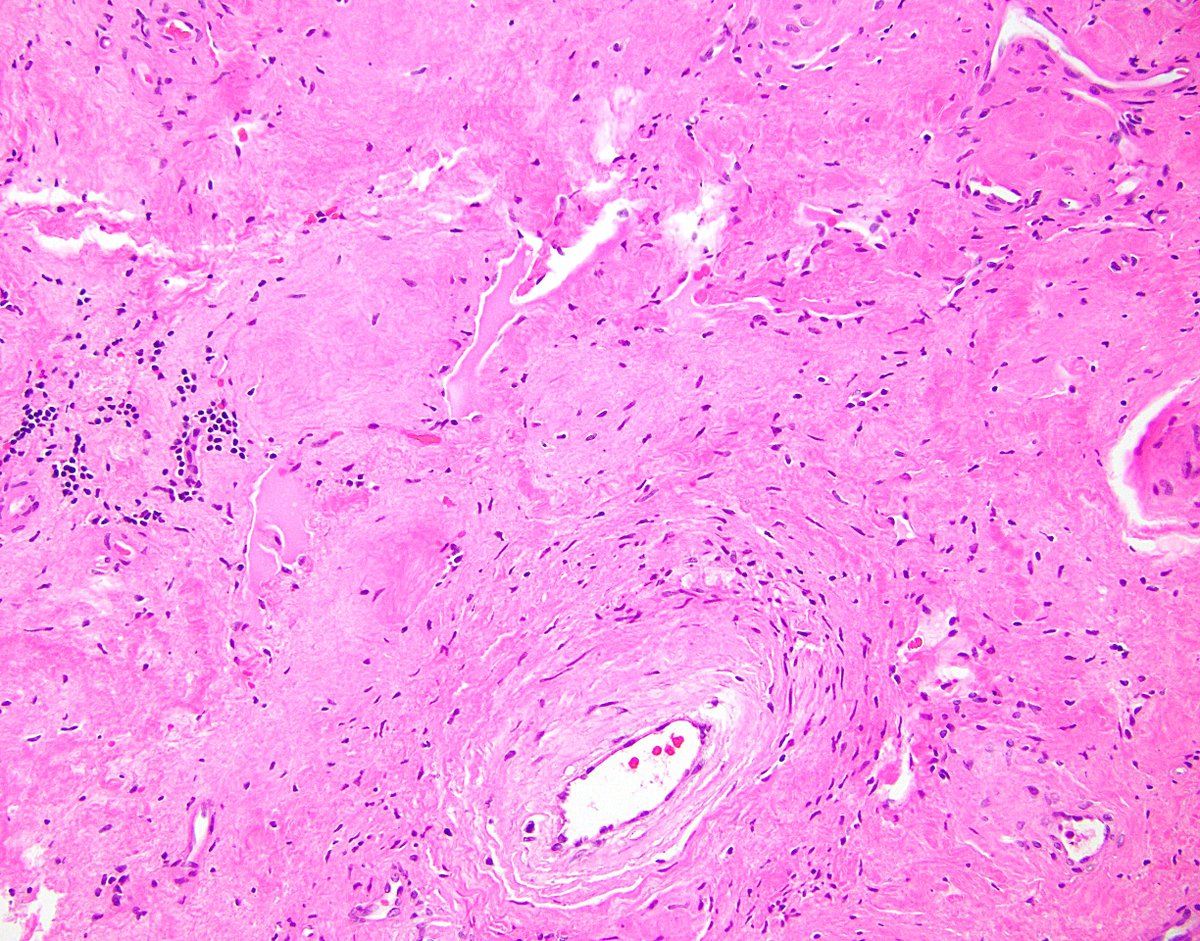
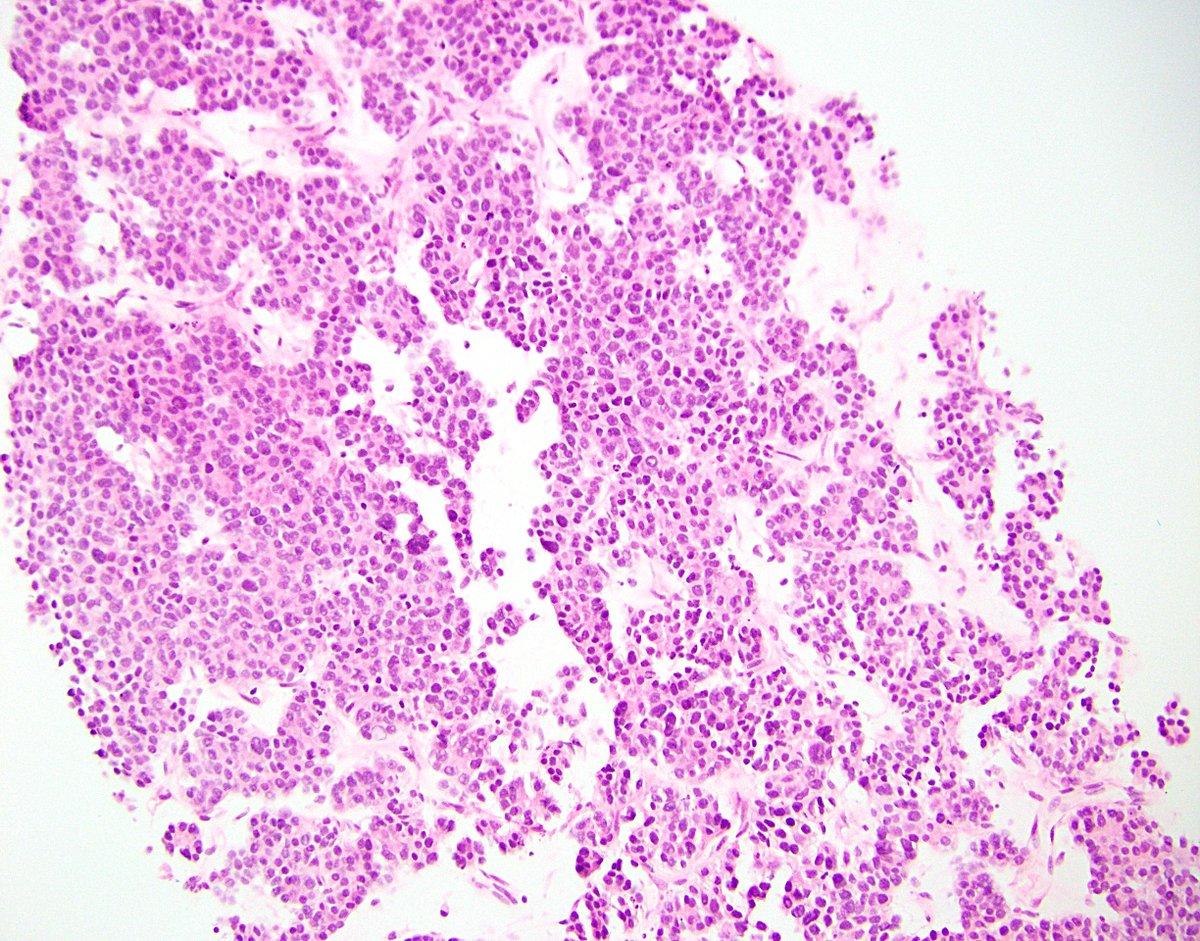
38/ Many histologic subtypes, including fetal (pic 1), embryonal (pic 2), mixed epithelial-mesenchymal (pic 3), and teratoid (pic 4). Pics 2-4 taken from the amazing resource @webpathology.
44/ There purportedly exists an aggressive lesion called transitional liver cell tumor. Extremely few cases reported, mostly in children. I’ve never seen one. I think some peds pathologists doubt it actually exists. It’s not in the new WHO.
54/ Finally, I’ll end with a curveball, because there’s always weird stuff to consider. This biopsy was from a case of what ended up being diagnosed as … primary acinar cell carcinoma of the liver? bit.ly
55/ And that’s my time! I hope everyone enjoyed my second Tweetorial, which was a whopping four tweets longer than my first. I may do a third one in the future, if I can find the time. So … maybe in another year? :)
Loading suggestions...