So it's time for #gijournalclub! Let the discussion begin on the recent @AGA_Gastro's paper on the long-term malignancy risk in IPMNs! Expert commentary by the excellent, Dr. @ShyamTMD!
@GiJournal @BilalMohammadMD @AHNtoday @letswinpc @RetePancreatic @PCE_Association @DeMadaria
@GiJournal @BilalMohammadMD @AHNtoday @letswinpc @RetePancreatic @PCE_Association @DeMadaria
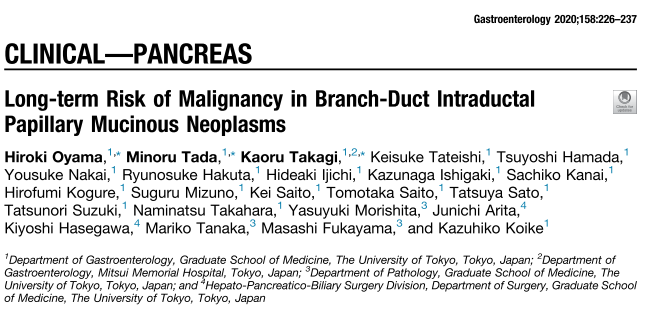
Introduction (1/3):
- IPMN of the pancreas has been recognized as a precursor
lesion of pancreatic carcinoma.
- The incidence rate of pancreatic carcinogenesis during follow-up has been reported to be approximately 3% to 8%.
- IPMN of the pancreas has been recognized as a precursor
lesion of pancreatic carcinoma.
- The incidence rate of pancreatic carcinogenesis during follow-up has been reported to be approximately 3% to 8%.
Introduction (2/3):
- AGA guidelines recommend discontinuing surveillance of asymptomatic pancreatic cysts with no or minimal change during a 5-year observation.
- AGA guidelines recommend discontinuing surveillance of asymptomatic pancreatic cysts with no or minimal change during a 5-year observation.
Introduction (3/3):
- Given the high mortality of patients with pancreatic carcinoma,12 there is a great need for the establishment of long-term surveillance programs for patients with branch-duct IPMNs!!
- Given the high mortality of patients with pancreatic carcinoma,12 there is a great need for the establishment of long-term surveillance programs for patients with branch-duct IPMNs!!
Patient and methods (1/2):
- Prospectively collected database.
- Included 1404 patients who were diagnosed with branch-
duct IPMNs from January 1994 to December 2017.
- Prospectively collected database.
- Included 1404 patients who were diagnosed with branch-
duct IPMNs from January 1994 to December 2017.
Patient and methods (2/2):
- Followed until the diagnosis of pancreatic carcinoma (IPMN-derived carcinoma or concomitant PDAC), death, or the end of follow-up, whichever came first.
- Followed until the diagnosis of pancreatic carcinoma (IPMN-derived carcinoma or concomitant PDAC), death, or the end of follow-up, whichever came first.
Ascertainment of Pancreatic Carcinoma Cases:
- EUS FNA +/- ERCP.
Analyses of Tumor Molecular Features:
- Mutation statuses of GNAS and KRAS.
- EUS FNA +/- ERCP.
Analyses of Tumor Molecular Features:
- Mutation statuses of GNAS and KRAS.
Results:
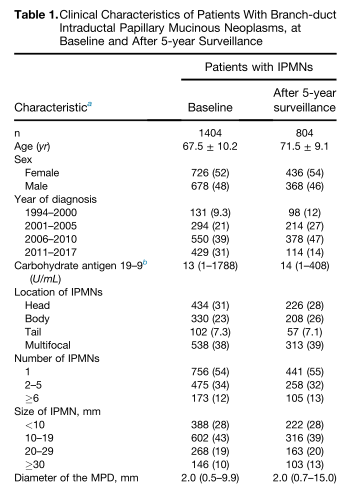
- Incidence of Pancreatic Carcinoma Among Patients With Branch-duct IPMNs: During follow-up of 1404 patients with branch-duct IPMNs (9231 person-years with median follow-up time of 6.0 years [range, 0.5–21.8 years]), we documented 68 patients diagnosed with PC!
- Incidence of Pancreatic Carcinoma Among Patients With Branch-duct IPMNs: During follow-up of 1404 patients with branch-duct IPMNs (9231 person-years with median follow-up time of 6.0 years [range, 0.5–21.8 years]), we documented 68 patients diagnosed with PC!
Results:
- The size of the IPMN and the diameter of the MPD were both associated with incidence of IPMN-derived carcinoma (SHR 1.85; 95% CI 1.38–2.48 for 10-mm increase, and SHR 1.56; 95% CI 1.33–1.83 for 1-mm increase, respectively).
- The size of the IPMN and the diameter of the MPD were both associated with incidence of IPMN-derived carcinoma (SHR 1.85; 95% CI 1.38–2.48 for 10-mm increase, and SHR 1.56; 95% CI 1.33–1.83 for 1-mm increase, respectively).
Results:
- Incidence and Risk Factors of Pancreatic Carcinoma Among Patients With Branch-Duct IPMNs After 5-year Surveillance: 819 (58%) patients with branch-duct IPMNs who were followed more than 5 years.
- Incidence and Risk Factors of Pancreatic Carcinoma Among Patients With Branch-Duct IPMNs After 5-year Surveillance: 819 (58%) patients with branch-duct IPMNs who were followed more than 5 years.
Results:
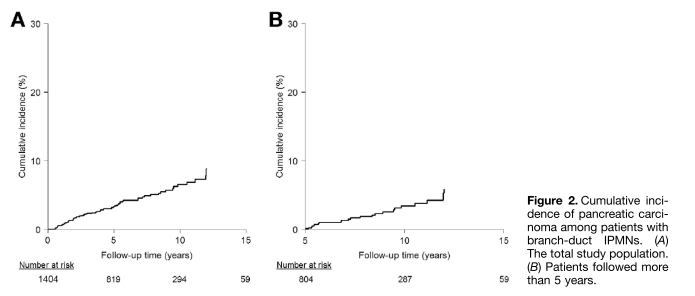
- During the follow-up of this subpopulation (3598 person-years with a median follow-up time of 3.9 years [range, 0.1–16.8 years] after 5 years), we documented 30 patients diagnosed with pancreatic carcinoma (IPMN-derived carcinoma in 16 and concomitant PDAC in 14)!
- During the follow-up of this subpopulation (3598 person-years with a median follow-up time of 3.9 years [range, 0.1–16.8 years] after 5 years), we documented 30 patients diagnosed with pancreatic carcinoma (IPMN-derived carcinoma in 16 and concomitant PDAC in 14)!
Results:
- As an exploratory analysis, we examined pancreatic carcinogenesis among patients with branch-duct IPMNs for whom discontinuation of surveillance at 5 years would be recommended according to the AGA guidelines.
- As an exploratory analysis, we examined pancreatic carcinogenesis among patients with branch-duct IPMNs for whom discontinuation of surveillance at 5 years would be recommended according to the AGA guidelines.
Results:
- We analyzed 737 patients with branch-duct IPMNs harboring up to 1 positive feature (ie, dilated MPD or size of IPMN greater or queal to 30 mm) at baseline and developing no additional positive feature during 5-year surveillance.
- We analyzed 737 patients with branch-duct IPMNs harboring up to 1 positive feature (ie, dilated MPD or size of IPMN greater or queal to 30 mm) at baseline and developing no additional positive feature during 5-year surveillance.
Results:
- In this subpopulation, we identified 23 patients diagnosed with pancreatic carcinoma, including 11 patients with IPMN-derived carcinoma and 12 patients with concomitant PDAC.
- In this subpopulation, we identified 23 patients diagnosed with pancreatic carcinoma, including 11 patients with IPMN-derived carcinoma and 12 patients with concomitant PDAC.
Results and Final slide:
- The cumulative incidence rates of pancreatic carcinoma were 3.2% and 9.5% at 10 and 15 years, respectively, from the initial diagnosis of IPMN. The SIR of pancreatic carcinoma was 4.8 (95% CI 2.9–6.8) during follow-up beyond 5 years!!!!
- The cumulative incidence rates of pancreatic carcinoma were 3.2% and 9.5% at 10 and 15 years, respectively, from the initial diagnosis of IPMN. The SIR of pancreatic carcinoma was 4.8 (95% CI 2.9–6.8) during follow-up beyond 5 years!!!!
So let us start the discussion with our Twitter audience!
So, we would like to welcome Dr. @ShyamTMD to our discussion! We appreciate your presence here @GiJournal! So tell us about the impact of this paper on your current clinical practice as an advanced therapeutic endoscopist and pancreatic cancer expert...
@ShyamTMD @GiJournal We would like to welcome Dr. @BilalMohammadMD as well to our discussion as an expert commentator! He is an extraordinaire advanced endoscopist fellow at @BIDMChealth under the supervision of @tberzin!
@ShyamTMD @GiJournal @BilalMohammadMD @BIDMChealth @tberzin Drs. @ShyamTMD and @BilalMohammadMD, with incidental imaging showing IPMNs in patients, this is becoming a more encountered issue in our practice. Were you feeling in a "grey area" when it was coming to stopping surveillance in surgically fit patients with stability over 5 years?
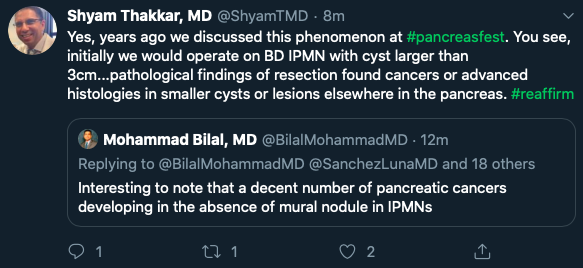
@ShyamTMD @GiJournal @BilalMohammadMD @BIDMChealth @tberzin Perhaps one of the most interesting findings, as discussed earlier with Dr. @ShyamTMD, the concomitant PDAC that some patients had! Would you agree with this, Dr. @ShyamTMD? Any thoughts on this as well, Dr. @BilalMohammadMD?
@ShyamTMD @GiJournal @BilalMohammadMD @BIDMChealth @tberzin And what is your current practice on sampling for KRAS and GNAS, Drs. @ShyamTMD and @BilalMohammadMD?
@ShyamTMD @GiJournal @BilalMohammadMD @BIDMChealth @tberzin As you both mentioned, @ShyamTMD and @BilalMohammadMD, the paper provides further understanding of the long-term risk! Now our job is to continue to be involved in shared decision-making so we provide the best care to our patients!
@ShyamTMD @GiJournal @BilalMohammadMD @BIDMChealth @tberzin And before the hour ends, I would like to deeply thank @SultanMahmoodMD and @ijlalakbar from @GiJournal for the kind invitation to moderate this session! Also, my deep gratitude to Drs. @ShyamTMD and @BilalMohammadMD for whom my gratitude extends beyond this journal club session!
Loading suggestions...